Delaying cord clamping until respiration is well established is a physiologically pleasing approach, and avoids the dramatic decrease in left ventricular preload, simultaneously with an increase in afterload that occurs with early clamping. But does delaying clamping during positive pressure ventilation have the same physiologic benefits? I had previously thought that the decrease in intra-thoracic pressure associated with an inspiratory effort might increase placental venous return, and that therefore positive pressure ventilation with the cord intact might not have the same benefits. That is probably wrong, although the differential effects of delayed cord clamping with spontaneous respiration and assisted ventilation are not clear to me.
What is clear is that positive pressure ventilation decreases pulmonary vascular resistance, although surprisingly, we don’t really understand the mechanism. Stuart Hooper’s group has done much of this work and in one fascinating study (Lang JA, et al. Increase in pulmonary blood flow at birth: role of oxygen and lung aeration. J Physiol. 2016;594(5):1389-98), they showed that positive pressure ventilation of one lung with nitrogen, causes improved lung perfusion, of BOTH lungs. This was a study in near term fetal rabbits who were instrumented during partial cesarean delivery with the cord intact, but the actual procedures and images were taken after cutting the cord. So it tell us about the physiology of PVR reduction during positive pressure ventilation, but not about other aspects of delayed clamping and ventilation.
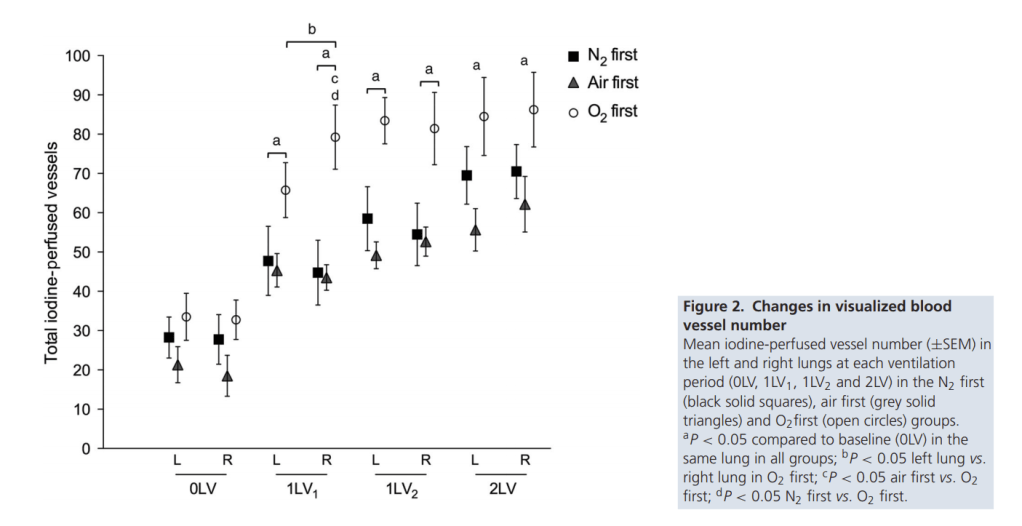
The fetal rabbit kits were ventilated unilaterally in the right lung with nitrogen or air or oxygen, then unilaterally with air (1LV2) then the tube was pulled back to ventilate both lungs with air. This is one selected image from the publication, showing the number of vessels that were seen in each lung, and that ventilating the right lung increased perfusion of both lungs, ventilating the right lung with oxygen increased perfusion further, especially of the right lung.
When you are doing physiologic studies in animals it is difficult to ensure that the animals make respiratory efforts reliably at the right moment, so most studies are about positive pressure ventilation. I guess in some ways it is less important for the future of delayed cord clamping what happens during spontaneous respiration, as it has become the standard of care to clamp the cord after at least one minute, if the baby is breathing. The responses to clamping before or after initiating PPV are of more relevance for the decision that we are still considering, whether we should routinely initiate PPV prior to cord clamping in depressed babies. The recent studies have not suggested any reason to me why we should clamp before PPV, if that is technically, logistically possible. In cases of an increased risk of needing PPV, I think the recent trial from Melbourne shows that it is not too difficult to get organized to do this. See the comment on my previous post from Doug Blank. (I’ve never linked to a comment before, hope that works).
I was thinking, based on the physiology, and the BabyDUCC trial, that we should all prepare to perform the initial steps of resuscitation during “natural cord management”. But hang on, what about an alternative… cord milking? (see next post!)









I see you still refer to ‘delayed’ clamping, when we should probably be considering it “an intervention without an indication”. What is the justification for ever clamping and amputating a functioning organ that is a baby-led reason rather than one to do with clinician convenience, custom and practice? I appreciate this change in focus is very difficult, but I do think its leading to more innovation in thinking.
So, how fascinating this work is! Whatever is happening in the one lung seems to have a systemic impact on both. If we don’t understand we risk making more clumsy manoeuvers that wont help as many babies as possible while we continue to pat ourselves on the back for ‘saving’ those babies who survive both despite and because of clamping before physiological ‘clamping/ closure of the placental circulations’. Babies might benefit from more of their own resilient ‘auto-ressusciation’, or they might benefit when there is some brain damage if they receive maximum numbers of stem cells concentrated in the last part of the transfusion….
Of course we should try to understand how to help the depressed baby (esp not making it worse), but can I ask how confident you are that any of us know what a third-stage depressed baby (ie still in an active maternal-fetal dyad) actually looks like? For all the attention she gave to the neonate, nevertheless it worries me a lot that the Apgar score was devised only on early clamped babies, and this may be why we really cant connect obstetric behaviour (based on appalling sensitivity and specificity of fetal monitoring) to early measures and later outcomes. Do we really know, and might we not have to start again, on ‘normal ranges’ of each of the parameters, teaching obs/ MWs & NNs to properly assess the situation prior to birth, and make observations like heart rate, colour, turgor and pulsation of the cord – obsessing less about the ‘score’, or first breath and cry (maybe precipitated by placental amputation) than a sequential unfolding of the transition.
Lastly, you say that “it has become the standard of care to clamp the cord after at least one minute, if the baby is breathing”. Are you sure this is happening in all births – and how do you know? And what about a healthy baby who doesn’t establish breathing immediately (having not breathed air for the last 9 months, why is it urgent?). Must the cord be clamped?
Thanks for the comments again, its hard to change the language that has been developed… I think it is “standard of care”, but that certainly doesn’t mean its always done! It has rapidly become the routine for vaginal and cesarean deliveries in our hospital, I am actually impressed how the ingrained reflexes of a life time of practice for many OBs have changed to a more natural approach over a short period of time.
There are a few babies every year in our practice that are born “flat” after an apparently low risk Cesarean, most respond to relatively simple manoeuvres, which are currently usually performed by the anaesthesia personnel, after cord clamping. I think OBs could easily do that in most circumstances, but need to be ready to do so, and we need to have back up if they are still working on the Mum.
Your comments about the Apgar score are about right, but we don’t use the score to decide on any part of resuscitation, I think we could easily junk the score with no real down side. Several investigators round the world (especially the Melbourne group and and several people previously working with that group such as Colm O’Donnell and Georg Schmolzer, and others from around the world, like Anup Katheria) are workign on trying to make our approaches more evidence based, and ensure that we only intervene when we need to. Several people have commented that one of the advantages of physiologic cord management (I got it right that time) is that it keeps the neonatal team away from the baby for a minute or so. Which might be an argument against special equipment, and tables and so on!