A new large RCT from PICUs in the UK randomly compared 2 saturation target ranges, 88-92 and >94%. (Peters MJ, et al. Conservative versus liberal oxygenation targets in critically ill children (Oxy-PICU): a UK multicentre, open, parallel-group, randomised clinical trial. Lancet. 2024;403(10424):355-64). Children <16 years of age being ventilated with supplemental oxygen were randomized within 6 hours of admission. The intervention stopped when the child was extubated. Primary outcome was “the duration of organ support” up to 30 days after admission. This was “a rank-based endpoint with death either on or before day 30 as the worst outcome (a score equating to 31 days of organ support), with survivors assigned a score between 1 and 30 depending on the number of calendar days of organ support received. Organ support … included respiratory support… cardiovascular support… and renal support. Other components of organ support included analgesia or sedation, exchange transfusion, neurological support, and metabolic support”.
2040 patients were randomized and data included for 1872 of them (more about that in a moment), half of the children were <1 year of age.
Differences in outcomes were small, but there was a reduction in the adverse primary outcome,
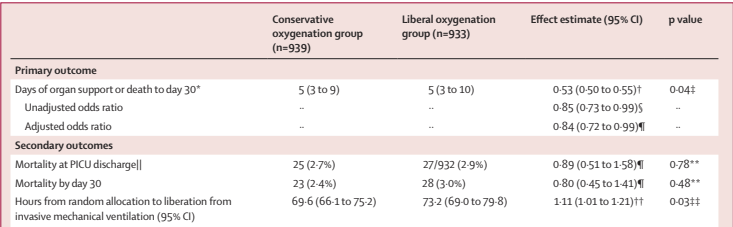
The size of the effect is expressed in a way which I find difficult to understand, it is “a probabilistic index of 0·53 (95% CI 0·50–0·55; p=0·04 Wilcoxon rank-sum test) indicating a higher probability for a better outcome in the conservative oxygenation group”.
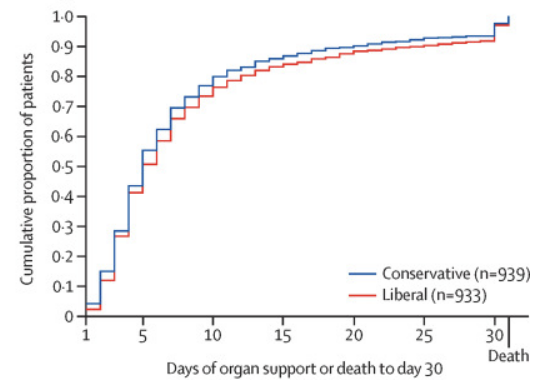
I found this graph made the results a little easier to comprehend, the cumulative proportion of infants in each group who required organ support in the first 30 days of hospitalisation, with the children who died scoring 31.
This relatively small advantage of lower SpO2 targets was achieved despite many infants being above the target range for significant periods of time. As in the preterm O2 studies, much of this is because they were in 21% oxygen, but some was due to periods of time in supplemental O2 with SpO2 above target.
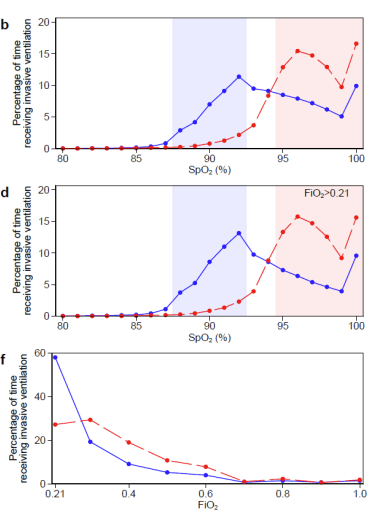
These 3 panels, using the same colours as the figure above, show the proportions of time by SpO2 in the top panel, the proportions of time with each SpO2 reading while receiving more than 21% oxygen in the middle panel, and the proportion of ventilated time with each FiO2 in the bottom panel. This is the version from the supplemental materials, which includes data up to day 30, data from the first 7 days are in the main article and look very similar. It looks like the lower SpO2 target group were extubated about 3 hours earlier on average, and may have had a shorter duration of cardiovascular support.
Previous studies in newborn infants of differing saturation targets include the early life trials which were meta-analysed in the NeoProm collaboration, and led to an increase in saturation targets, as mortality was higher with SpO2 targets in the high 80’s compared to the low 90’s.
Studies in older preterm newborn infants include STOP-ROP, and the first BOOST trial. STOP-ROP was a large RCT, published in 2000, among about 600 preterm infants who had developed pre-threshold retinopathy, as then defined, and who had a median SpO2 of <94% in room air. Pre-threshold was any zone 1 RoP of stage 1 or 2 without plus, or zone 2 RoP of stage 2 with a limited region of plus disease, or stage 3 without plus. The infants were randomized to target SpO2 in the low 90’s or the high 90’s (89-94 vs 96-99%), the idea being that some animal models showed decreased progression of retinopathy, after it had first appeared, when saturations were maintained in a higher range. It was thought that maintaining retinal ateriolar vasoconstriction with mild hyperoxia could prevent neovascularization. There was no overall difference in ophthalmic outcomes between groups, on subgroup analysis there might have been an advantage of the high oxygen group in the eyes that did not have plus disease, but the most severely affected infants, with plus disease, had no difference between groups. The intervention continued for at least 2 weeks, and until the baby’s eyes had either reached “threshold” (and treatment indications) or had shown regression on 2 subsequent eye exams. Almost all the babies were out of the study before discharge, as they had satisfied eye end points. Babies were usually randomized at about 35 weeks PMA, and therefore most had a BPD diagnosis. All the pulmonary outcomes were worse in the group with higher SpO2 goals. There were more babies still hospitalised at 3 months corrected age, more babies on oxygen at 3 months, were more episodes of pneumonia and episodes of BPD exacerbations in the supplemental oxygen group. In contrast to the expectations of the investigators, babies with higher oxygen saturations did not grow any better, with identical weight gain between groups.
BOOST was a trial from Australia of supplemental oxygen among 360 preterm infants <30 weeks GA who had reached 32 weeks and still required oxygen. They were randomized to target SpO2 of 91-94% or 95-98% (using masked oximeters) and remained in their group until oxygen was stopped (including when at home). The hypothesis behind this trial was also that higher saturations would lead to better growth and development, which was a reasonable supposition, based on observational data that babies who had been maintained with higher saturations had better outcomes in those domains. The RCT, in contrast to the observational data, showed no advantage in growth or development. In order to maintain the higher saturation, the high SpO2 group stayed in oxygen much longer, and were more likely to go home in oxygen. They also had more respiratory related deaths (1 vs 6, p=NS), more treatment with steroids and/or with diuretics, and had more re-hospitalisations.
Which suggests that even small increments of inhaled oxygen concentrations can have pulmonary toxicity, and that the balance between ensuring adequate oxygen delivery while limiting oxygen-induced lung injury is a very narrow one. Maintaining tight oxygen saturation limits, and avoiding even mild hyperoxia seems to be important for ensuring the best clinical outcomes, in older children, as well as in newborn infants.









Thanks for the interesting information about oxygen in PICU. Could you please share a link to the publication?
Oops! here is the link https://pubmed.ncbi.nlm.nih.gov/38048787/ I have also edited the post to include the reference and the link. Thanks
And cohort data from CNN, comparing targets 88-93% (non enrolled arm in COT; units which did not change targets/alarms) and 90-95% ( “higher” targets, mostly with higher alarms) show no improvement in NEC or mortality with higher targets but a decrease in survivial at discharge free of morbidity – mostly due to higher BPD with higher targets….
We still dont know the answer, but we are getting there!
currently this study is taking place in The Netherlands, also looking at different saturation targets in neonates with esthablished BPD and growth as the primary outcome.
https://pubmed.ncbi.nlm.nih.gov/35803625/