Progesterone analogues, including 17-OH progesterone caproate have been investigated over the last several years for prevention of prematurity. In the pivotal trial from 2003 17OHPC intramuscularly once per week was shown to reduce prematurity at less than 37 weeks, less than 35 weeks (from 31% to 21%) and less than 32 weeks, and to reduce complications of prematurity (NEC and IVH).
Since then the literature has been a bit mixed, with many studies of different ways of administering progesterones being performed, many with daily vaginal pessaires, and some with oral administration, as well as others with the 17OHPC. Many studies among different groups at risk of prematurity have been positive (twins, short cervix, early cervical dilatation, premature rupture of membranes) but a few have been negative, and many small underpowered trials have appeared.
The newest trial was an attempt to reproduce the first Meis trial (Blackwell SC et al. 17-OHPC to Prevent Recurrent Preterm Birth in Singleton Gestations (PROLONG Study): A Multicenter, International, Randomized Double-Blind Trial. American Journal of Perinatology. 2019). An international RCT was performed with nearly 3 times the sample size of the previous study (n=1700), admission criteria were similar to Meis; that is a mother with a previous spontaneous preterm birth (with or without earlier rupture of membranes), and pregnant again with a singleton between 16 and 20 weeks of gestation.
Despite similar criteria for enrolment the actual placebo group rate of prematurity was much lower than Meis et al, at 11.5%. The intervention was identical, with 17OHPC weekly, and the outcome variables were also similar. The treatment group rate of prematurity < 35 weeks was practically identical to the controls, at 11.0%, that is there was no apparent treatment benefit.
Following this new trial an advisory committee of the FDA has recommended that the licence of 17OHPC be revoked in the USA. The submission of Public Citizen to that committee follows their tradition of brain-dead comments on pivotal perinatal trials. They state that the Meis trial was “seriously flawed”, but the only thing they note to support this statement is that an FDA statistician had stated that there wasn’t a second confirmatory study. No other “serious flaws” are described, and they quote the statistician as saying “The results of the analyses of the 32 and 35 week endpoints suggest their false positive rates could be as great as 1/40”, which is of course substantially better (p<0.025) than the 1/20 false positive rate that is usually required!
What about other trials? There are many systematic reviews covering various aspects of progesterone use. A network SR and meta-analysis was published this year (Jarde A, et al. Vaginal progesterone, oral progesterone, 17-OHPC, cerclage, and pessary for preventing preterm birth in at-risk singleton pregnancies: an updated systematic review and network meta-analysis. BJOG. 2019;126(5):556-67).
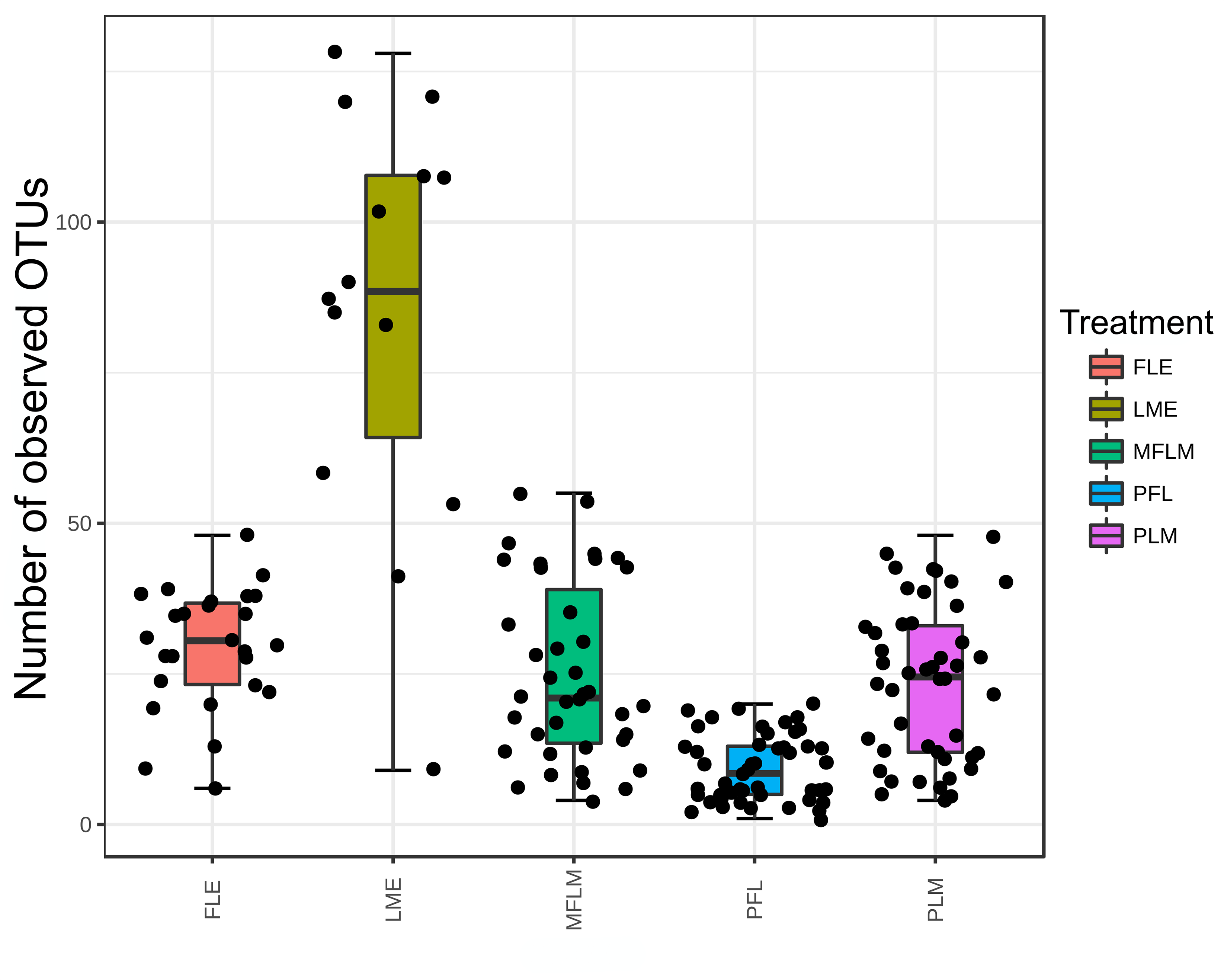
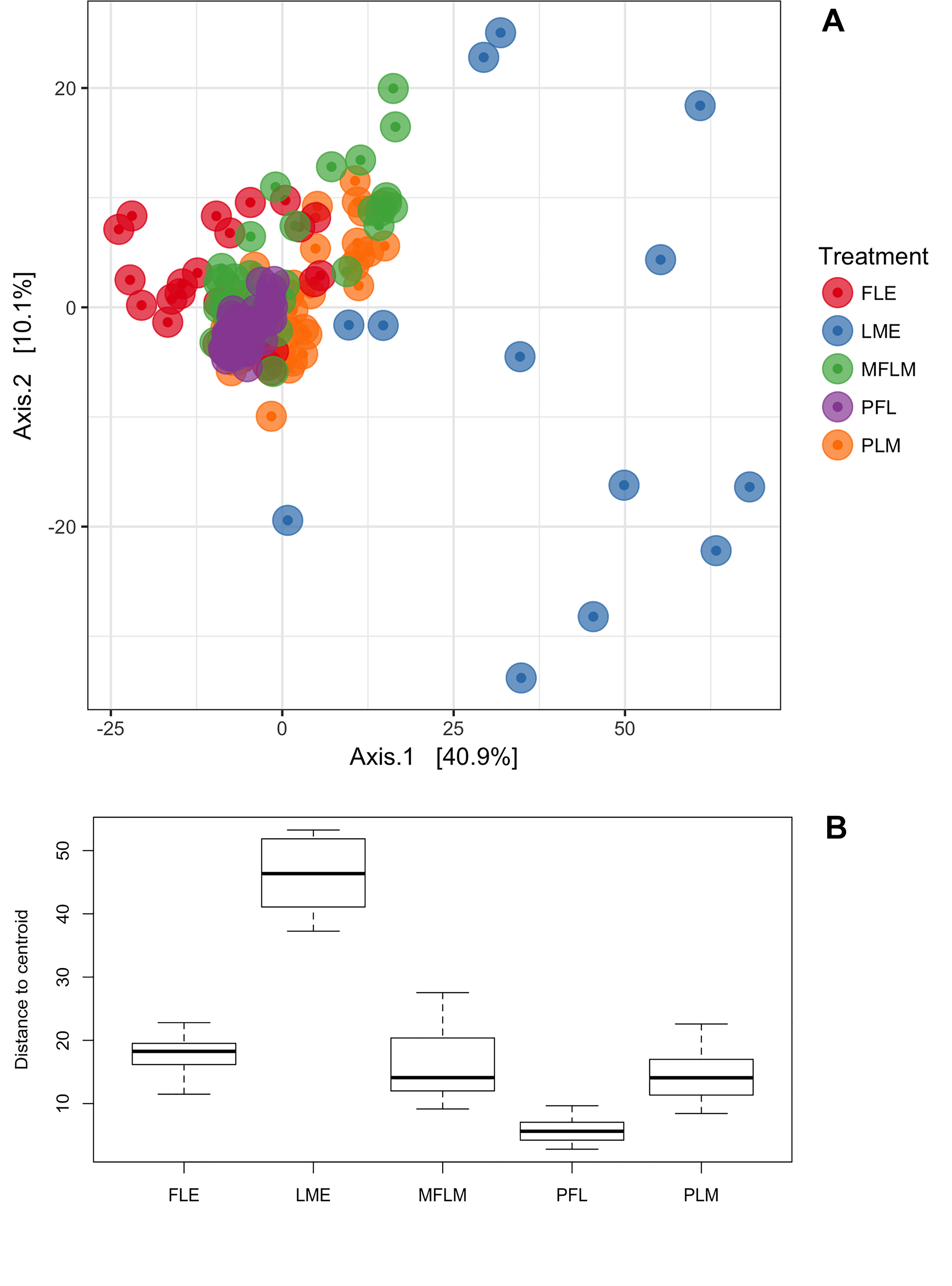
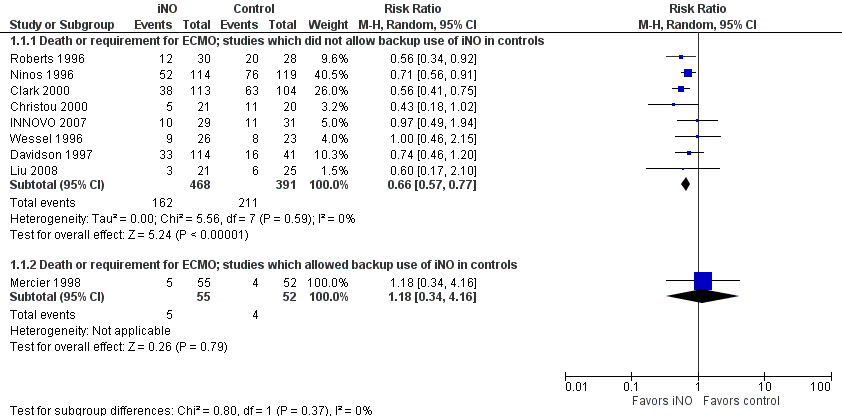
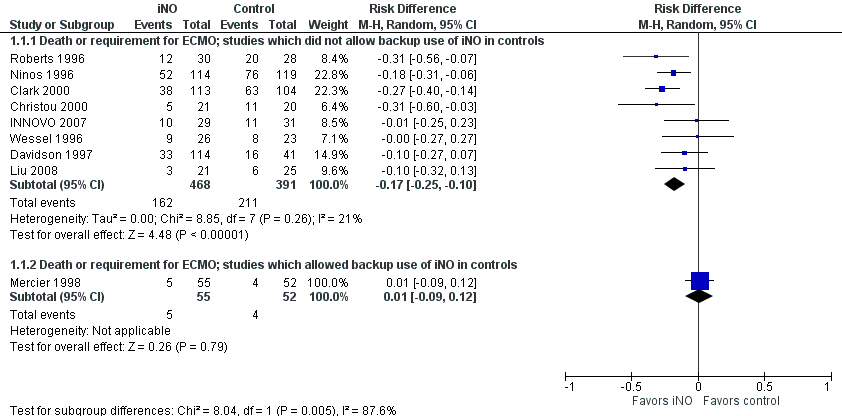
This was the result of the meta-analyses of delivery before 37 weeks. The earlier threshold chosen for this review was 34 weeks, and, for the 17OHPC, Meis reported prematurity <35 and <32 weeks, so the meta-analyses for delivery <34 weeks has very few patients, and doesn’t include Meis, it is basically just the Grobman trial which showed a small reduction with the drug.
As you can imagine the authors of the new trial were a little perplexed at the lack of effect, given the prior data. One of their suggestions is that, given the prior data regarding benefits of progesterones, many physicians were already prescribing them to the highest risk patients, and those who remained to be randomized had a much lower rate of premature delivery, which reduces power and perhaps selects a group with less progesterone responsiveness.
It remains a possibility of course that 17OHPC is not a very effective method of getting progesterones into mothers, and that the benefits shown in the Meis trial were indeed a “false positive”. Perhaps by chance they enrolled a control group which had a much higher rate of preterm delivery than the treated babies (which is a possibility but is unlikely), or perhaps there was some other bias in the study design, but I can’t see one.
Of course, it is also possible that the new trial is a false negative, the 95% compatibility intervals for the relative risk of preterm delivery before 35 weeks include the possibility that there is a 29% reduction (or indeed a 26% increase) in this outcome.
To keep this all in context of the entire literature about progesterones for preterm delivery, the comparative trials of vaginal progesterone and 17OHPC seem to show that the vaginal progestrone is the more effective of the 2, but includes numerous small trials and a couple of more moderately large trials, as you can see in the figure above. It is a treatment which has the advantage of avoiding weekly IM injections also. However, the confidence intervals are wide and only one individual trial showed a meaningful difference between the interventions, also the majority of the trials were unmasked, so the confidence in the advantage of vaginal progesterone is very low.
In fact if you critically look at the vaginal progesterone vs placebo trials it is only the smaller trials that show benefit, the 3 larger trials, Crowther, O’Brien and Hassan, don’t show very much.
I think the best way to settle this would be…. (drumroll…) another trial! I think that, in an ideal world (with very compliant mothers) we would perform a very large 3 arm trial with vaginal progesterone plus IM placebo, vs vaginal placebo plus IM 17OHPC, vs vaginal placebo plus IM placebo.
That won’t happen! So what could reasonably be done? I think it is probably inappropriate to take 17OHPC off the market; as well as the evidence of efficacy from one high quality trial with very high prematurity rates in both arms, there has been no real evidence of adverse secondary effects in any of the trials, including in long term baby follow up. Maybe this new trial will create enough uncertainty that a simpler trial than the one I suggested above could be performed, and try to enroll the highest risk mothers, but I am at a loss really.
The more I read about these trials, the more confused I get, and I end up being unconvinced by any of the data. The best 2 trials of all, I think, are Meis and the new Blackwell trial, and they come to different conclusions!