Following on from the previous post:
This all brings me to a larger and very thorny issue, which is whether we should even be routinely starting parenteral nutrition (PN) immediately after birth at all! I hate to discuss this, as I will probably sound like a Luddite wanting to destroy the new-fangled mechanical looms that everyone knows are the future.
As mortality rates were progressively decreasing during the early development of neonatal care we assumed that everything we were doing was good (and most of it was, apart from a series of serious errors, hyperoxia, hexachlorophene, chloramphenicol, benzoic acid…). However, many innovations that were introduced were not subject to adequate scientific investigation. There were some innovations, such as the introduction of CPAP and PEEP, that led to immediate survival of babies who would previously have died, and did not require further testing. Some innovations such as early PN, which was initially accompanied by periods of prolonged fasting of very preterm babies, have never been well enough studied.
Immediate PN in the very preterm baby has been promoted (by me, among others) as a way of minimizing the otherwise dramatic nutritional deficits which arise in the early life of the very preterm infant. Very preterm babies have such low fat and protein content, and high metabolic demand, that they become catabolic quickly after birth. This catabolic phase can be eliminated with early parenteral nutrition (PN). Surely that is a good thing! Most of the trials of early PN have focussed on different components, different doses of protein etc. and they have mostly examined short term metabolic impacts, such as changes in protein balance. Whether we should really be doing this at all has not been well studied.
One study that made me pause and think about this was the PEPaNIC trial (Fivez T, et al. Early versus Late Parenteral Nutrition in Critically Ill Children. NEJM 2016;374:1111-22) this was a study from Europe and Canada that randomized children in the ICU to either immediate PN, or to wait 7 days before starting PN. Infants in the early PN group were much more likely to develop sepsis. It would be easy to say that this was older children of many different pathologies, and has limited relevance to the NICU, but there was a pre-planned subgroup analysis of the full-term babies involved. The initial publication of the trial of 1440 children in PICUs showed the following :
new infection was 10.7% in the group receiving late parenteral nutrition, as compared with 18.5% in the group receiving early parenteral nutrition (adjusted odds ratio, 0.48; 95% confidence interval [CI], 0.35 to 0.66). The mean (±SE) duration of ICU stay was 6.5±0.4 days in the group receiving late parenteral nutrition, as compared with 9.2±0.8 days in the group receiving early parenteral nutrition; there was also a higher likelihood of an earlier live discharge from the ICU at any time in the late-parenteral-nutrition group (adjusted hazard ratio, 1.23; 95% CI, 1.11 to 1.37). Late parenteral nutrition was associated with a shorter duration of mechanical ventilatory support than was early parenteral nutrition (P=0.001), as well as a smaller proportion of patients receiving renal-replacement therapy (P=0.04) and a shorter duration of hospital stay (P=0.001).
More of the late PN group had a hypoglycemic event (9% vs 5% had blood sugar less than 2.2 mM/L (=40 mg/dL)), but apart from that all of the differences between groups were in favour of the late PN group.
The newborn group from that trial was analyzed separately (van Puffelen E, et al. Early versus late parenteral nutrition in critically ill, term neonates: a preplanned secondary subgroup analysis of the PEPaNIC multicentre, randomised controlled trial. Lancet Child Adolesc Health. 2018;2(7):505-15). I must say I am really pissed off that even 2 years after this was published it is still not open access. Even with my good fortune as a professor of paediatrics at the University of Montreal and our inter-library loan system, I still cannot get immediate access to the full text of this study. The Lancet group of journals, which includes the journal which published this article, asks for at least $22 (Canadian) to have short term access to the full text. The research was performed using public money (European money, but still), and now to see the results I have to spend my own cash! Thankfully the authors have been very helpful and sent me a copy of the pdf immediately when I asked.
There were 209 newborns in the PEPaNIC trial, 98 in the early PN group and 110 in the late group. Of those 145 were 1 week or less of age, and 45 were on day 1 of life. They were in the PICU rather than an NICU mostly because of a surgical diagnosis, including cardiac surgery; that applies particularly to the babies under 1 week of whom over 80% were surgical. The main comparison in the trial is described here:
For patients assigned to early parenteral nutrition, this was initiated within 24 h after admission to the paediatric ICU as supplementation if enteral nutrition provided less than 80% of the target to reach the local age-specific and weight-specific caloric targets. In patients assigned to late parenteral nutrition, parenteral nutrition was withheld during the first week in the ICU. To match the fluid administration of the early parenteral nutrition group, taking into account the volume of enteral nutrition delivered, a mixture of dextrose 5% and saline was provided. To prevent refeeding syndrome, patients from both groups received intravenous micronutrients (trace elements, minerals, and vitamins) early in similar amounts, until enteral nutrition reached 80% of caloric targets. For patients from both groups who were still in the ICU after a week and who were not yet receiving 80% of the caloric target enterally, parenteral nutrition was administered to reach the targets.
The two primary end points were new infection acquired during the ICU stay and the duration of ICU dependency, which was adjusted for five prespecified baseline risk factors (diagnostic group, age group, severity of illness, risk of malnutrition, and treatment center)
Among the newborn infants, just as for the overall study group, there were many more hospital-acquired infections when the babies received early PN, compared to PN not started until 1 week. 31% vs 16% for the whole newborn group, the younger the babies were at admission, the more striking the difference between groups. Under 1 week it was 36% vs 14%, and in the day 1 babies, the difference was 57% vs 12%. The early PN babies also had longer ventilator dependence, longer PICU length of stay, which continued to be different after adjustment for potential confounders.
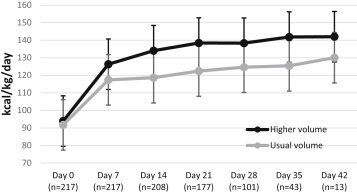
The newborn subgroup was more likely to have at least one blood sugar <2.2 mM/L in the late PN group. As you can see from the supplementary tables (well you can’t actually because you have to pay for them also so I’ll copy one example here) the late PN group had much lower intakes of sugar, protein and fat during the 1st week, the 1-day olds were almost all nil by mouth, it seems, as their enteral nutritional intakes averaged 0.
You can see from this table showing the nutritional intakes of the babies admitted on day 1 that the parenteral glucose intakes were very low in the late PN group; probably using 10% dextrose, instead of 5%, and ensuring adequate glucose intake to prevent hypoglycaemia would be preferable. 
A further secondary analysis of the results in this subgroup (and it is now starting to get risky, secondary analysis of one facet of the intervention in a subgroup, addressing the 2 primary outcomes and one secondary outcome) suggested that the main culprit was the amino acids
In neonates aged up to and including 4 weeks, higher average doses of aminoacids were associated with a lower likelihood of earlier live discharge from the paediatric ICU from day 2 to day 5 (HR 0·56–0·71, p≤0·04). In neonates aged up to and including 1 week, a similar association reached significance for doses up to days 3, 4, and 7 (HR 0·42–0·70, p≤0·04; figure). Higher average doses of aminoacids were also associated with a lower likelihood of earlier live weaning from mechanical ventilation from day 3 onwards in neonates aged up to and including 4 weeks (HR 0·44–0·66, p≤0·01; figure). A similar association with aminoacids occurred in neonates aged up to and including 1 week, with significance reached for average doses administered up to days 4, 6, and 7 (HR 0·32–0·58, p≤0·03; figure). No association occurred between the average doses of glucose and any of the efficacy endpoints. Higher average doses of lipids were associated with a higher likelihood of an earlier live discharge at day 7 in both neonates aged up to and including 4 weeks (HR 1·66, 95% CI 1·11–2·52; p=0·015) and aged up to and including 1 week (2·00, 1·15–3·45; p=0·013). Higher average doses of lipids were also associated with a higher likelihood of an earlier live weaning from mechanical ventilation in neonates aged up to and including 4 weeks (up to days 6 and 7, HR 1·46–1·73; p<0·05) and those aged up to and including 1 week (up to day 7, HR 2·10, 95% CI 1·17–3·93, p=0·016; figure).
The “figure” referred to is the following, which I found somewhat confusing. It suggests that none of the individual components of the PN were associated with nosocomial infections, which is weird.

Figure: Association of average total macronutrient doses in each of the first 7 days in the paediatric intensive-care unit with clinical outcome Data are hazard ratios (HR; 95% CIs) per g macronutrient/kg added. The figure shows associations of average daily doses of the individual macronutrients up to each of the 7 days with the likelihood of (A) acquiring a new infection in the paediatric intensive care unit, (B) earlier live discharge from the paediatric intensive care unit, and (C) earlier live weaning from mechanical ventilation. Results were obtained after adjustment for centre, paediatric logistic organ dysfunction score, paediatric index of mortality 2 score, diagnosis group, and weight-for-age Z scores on admission. HR >1 indicates a higher likelihood of acquiring a new infection (indicating harm), but a higher likelihood of earlier live weaning from mechanical ventilation and earlier live discharge from the paediatric intensive care unit (indicating benefit) and vice versa for HR <1. N represents the number of patients still in the paediatric intensive care unit on the day of analysis. The dotted lines represent a neutral relationship in form of hazard ratios being equal to 1 (border between harm and benefit).
I think it would be a mistake to assume that this means that lipids and glucose were beneficial. The babies on early PN almost all received both amino acids and lipids, and it is only by this data dredging, which might be suggestive but is certainly not conclusive, that the potential relatively different impacts of different components of the PN can be seen.
One strange thing about this trial is the infection outcome data, a 57% incidence of PICU acquired infection in full term babies seems enormously high, (16/28 1 day old babies in the immediate PN group). If you examine the tables the numbers of individual types of infection don’t add up to the total number of infections among the under 4 week and under 1 wk tables, even though there is a group called “others”.

Until the last few years I was starting PN immediately in the preterm infant, but I was willing to wait a few days in term babies, usually only starting the PN if they were likely to be without feeds for 3 or 4 days or more. Like many people I guess, as a result of indication drift, we now often start PN on day 1 when we admit term babies to the NICU.
We should rethink that approach. There may be no benefit to early PN in term babies apart from reducing hypoglycemia, which you can avoid with more glucose. An RCT of lipid and glucose vs glucose alone vs PN in babies expected to need less than 1 week of nil by mouth would be needed to really answer the questions in term babies. I think we really need to study this in NICUs where hospital-acquired infections among full-term babies are very much rarer than the figures in either group in PEPaNIC. In the latest CNN report the rate of late-onset sepsis among full-term babies admitted to the NICU was 1%. Of course, this is in no way comparable to the population studied in PEPaNIC, but it does make me wonder why so many of their babies developed infections, in both the early and the late PN group.
In the supplementary data, there are some tables examining risk factors for infections. Including this one for example which shows that the Odds Ratio for developing an infection were 0.0 in Edmonton, which I presume means that they didn’t have any. I don’t understand how the p-value for that can be 1.00, maybe there is an error there, or I am just not understanding. It is also possible that the definition of “airway infection” is the cause of the high frequency, and perhaps the cardiac surgery babies are at enormously high risk of satisfying that particular definition.

And what about the preterm? The nutritional fragility of the preterm, especially the very preterm, and preventing or reducing the usual protein catabolism after birth, has been the justification for the immediate introduction of PN. What if that is the wrong approach? The trials of earlier aggressive PN have I think not been adequately powered to answer questions of clinically important outcomes. The NEON factorial trial from the UK is one of the better ones, but even that only included outcomes of 133 babies of <31 weeks who either received high immediate amino acid intakes (3.6 g/kg/d) or a gradual increment, 1.7, 2.1 then 2.7 g/kg/d, which also started on day 1. The other arm of the factorial was comparing 2 different lipid emulsions, both arms of which received 2 g/kg/d on day 1 and 3 g/kg/d on day 2. The primary outcome for the amino acid arm was lean body mass at term equivalent which was not different between groups. Among secondary outcomes, the early higher dose AA group had smaller head circumference at term by 0.8 cm, but had slightly higher brain volumes on MRI.
I think it is important that we gain better information about the clinical outcomes of babies who receive early PN.
I suggest we obtain some observational data to start with (already underway in the UK) and then perform RCTs in full-term babies in the NICU, as suggested above we could have a group that just received extra calories as lipid. Then mildly preterm babies, and depending on those results we could consider studying moderately or very preterm infants. Early PN reduces or prevent catabolism in preterm babies, we should figure out whether that leads to better short, medium, or long term outcomes.