For a pre-christmas present, one of the most important recent studies in neonatology.
The study is related to the following question: if I wanted to know how best to counsel my very preterm baby parents about potential long-term outcomes, when they were ready to go home, how should I do this?
Should I have an MRI for all of them, then talk about the results? Is a head ultrasound just as good? Perhaps imaging is not very accurate as a predictor and I should just examine the baby and summarize his clinical course?
The team from “the centre for the developing brain” in London, led by David Edwards, performed this landmark randomized controlled trial. (Edwards AD, et al. Effect of MRI on preterm infants and their families: a randomised trial with nested diagnostic and economic evaluation. Archives of disease in childhood Fetal and neonatal edition. 2017).
They enrolled over 500 babies who were born before 33 weeks gestation in several London hospitals. All the babies had a head MRI and an ultrasound at around term equivalent (38 to 44 weeks) at a single expert centre.
They were then randomized to receive the results of either one or the other test. The results were explained to them by an experienced physician who showed them the images, gave them a copy of some pictures and discussed the developmental prognosis. For the ultrasounds they discussed the prognosis using data from their own systematic review of the prognostic accuracy of head ultrasounds for prediction of cerebral palsy, and only when there was a lesion present with a positive predictive value of more than 25%. They don’t say exactly the same thing for the MRI, giving instead the reference to Woodward’s study from the NEJM in 2006; which was a study that did not calculate the PPV of the abnormal findings. I presume they were presenting the MRI results as being adverse, and predictive of an abnormal outcome, when they showed moderate to severe white-matter abnormalities. In that study there were 35 babies (of 167 total) who had moderate (29) or severe (6) white matter abnormalities. Of whom 7 and 4 developed cerebral palsy of any degree (the GMFCS system was not used). If we use those CP numbers to calculate the Positive Predictive Value of the term-equivalent MRI it works out to 31% (11 of 35) in the cohort of Woodward et al for moderate or severe findings.
In this new publication, there were 72 babies who had MRI findings considered to predict a poorer outcome, and 22 with ultrasound findings that were considered predictive.
The study wasn’t designed this way but I would be very interested to see what happened to the families who had ultrasound findings not considered predictive, but MRI findings which were…
What the authors did actually do was to present the results of the un-masked test to the families. This was done as follows “An experienced physician unaware of the unallocated result discussed the allocated images and neurodevelopmental prognosis in a structured interview with parents, providing permanent examples of the images and a written summary of the prognostic information”. The “structured interview” by an experienced member of this group, among the world’s experts in evaluation and interpretation of imaging findings in such patients, would have been very interesting to see more details about.
What should we say to parents when we have the results of a test with very poor positive predictive value for adverse outcomes, but relatively good negative predictive value? When the prevalence of that adverse outcome is relatively low? By which I mean that 92% of the infants in this study did not have CP with a GMFCS of 2 or more, similar to data in many other studies; if you have a normal pre-discharge MRI that increases to about 96%, (based on previous publications) a modest improvement in NPV over not doing an MRI, but still not to 100%.
I guess you would have to say something like “your baby has an imaging study which is normal/abnormal, which doesn’t have much impact on our prediction of their long-term outcome. He/She will be followed-up with frequent evaluations, and we expect that things will go well. There is a small chance of developing problems with control of movement, and your baby will be examined so that if something develops they can get any therapy that they need. There is about a 1 in 3 chance of a delay in language development, and a 1 in 5 chance of overall slower than average development, we will be doing testing to see if those things happen and can offer support and intervention if they do turn out to occur.”
I think you could say almost exactly the same thing to parents whose baby had an “abnormal” or “predictive” result on MRI or on ultrasound as you would say when the imaging does not show such abnormalities.
I don’t know what was said to the parents in this study, but they did not have an increase in their anxiety scores after the interview, indeed the scores went down a little in both groups. Anxiety scores were in fact the primary outcome variable of this study. The score used has a scale for “state”, that is how anxious you are feeling right now, and “trait”, that is how anxious you are in general over a period of time. Higher scores reveal more anxiety, and various cutoffs have been suggested as indicating clinically important anxiety, such as over 39 for young adults to over 55 for geriatric patients, the minimum score possible is 20. A previous study of parents with a baby in the NICU showed trait scores averaging in the low 50’s.
In this study the mothers’ “state” anxiety scores were slightly higher in the ultrasound group before the imaging visit (by about 0.8 points), and stayed slightly higher (by about 1.5 points) throughout the follow-up to 18-24 months. A difference which was not likely due to chance (p=0.02). The “trait” anxiety scores were more similar between groups, and the fathers’ scores were not different between groups.
In other words, with a structured explanation of the results from an experienced individual who understands the limitations of the imaging tests, there is no adverse impact on anxiety. Both MRI and US were followed by a small decrease in anxiety, a decrease which was slightly greater in the MRI group.
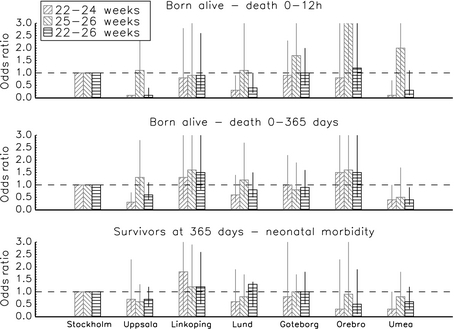
But were the tests actually useful? Were they actually predictive of long-term problems, based on Bayley version3 testing and neurological examination at 18 to 24 months corrected age? Here is table 4 from the publication showing the sensitivity, specificity and predictive values of MRI and ultrasound findings.

What they show basically is that the MRI finds more abnormalities, many of which are not associated with long-term problems, but some are. So the sensitivity of MRI is higher for all of the outcomes (but still relatively lousy, ranging from 18% to 60%) compared to head ultrasound (where they range from 5% to 16%), but the specificity is lower, around 90% for each outcome compared to around 97% for head ultrasound.
I think for an individual family the most important metrics are the predictive values, and, because of the increased details and increased detection of white matter abnormalities, the positive predictive values of an abnormal MRI are truly pathetic: from 28% to 48% for cerebral palsy and various components of the Bayley scores. The PARCAR-R test is a parent report of children’s abilities (revised), a parental questionnaire assessment which does not have the same standardization as the Bayley scales (i.e. it doesn’t have a mean of 100 and an SD of 15 in a standardized population), but a cut-off of 49 has been associated with a reasonably good distinction between infants with and without developmental delay, MRI had a very low sensitivity for this outcome, but was fairly specific, leading to a higher PPV but a low NPV. The M-CHAT is a screening test for autism features, which is affected by language delay; the MRI and the ultrasound prediction of failure on 2 or more items of the M-CHAT were quite similar to the results for prediction of language delay.
The authors of this article calculate the area under the receiver operator characteristics curves, which were modestly higher for MRI than for US for prediction of moderate or severe motor dysfunction (0.74 compared to 0.64) and for motor dysfunction, but were very similar for cognitive and language dysfunction.
Finally they calculated costs, and the MRI cost about 300 pounds stirling more than the US.
I think this study confirms my prior evaluation of the usefulness of brain imaging at discharge of the very preterm baby. Sensitivity is poor for any modality of imaging. Specificity is higher for ultrasound, but is problematic for MRI.
Dr Edwards group and the developing human brain project (and other projects around the world) are incredibly important programs aimed at understanding how the human brain develops, and what can go wrong, so that eventually we will be able to figure out how to normalize brain development in more infants, term and preterm.
See these amazing images, for example, from the King’s College London human connectome project:

These are 3-D reconstructions of the cortical surface of newborn brains, with the images showing the surface of the white matter at the top, of the grey matter next, followed by the inflated surface (whatever that means) different structures, sulcal depth maps, brain curvature, cortical thickness and T1/T2 myelin maps. You can see the progression of complexity and maturation of the brain in the last 8 weeks of pregnancy.
Their detailed connectome images from developing brains are stunningly beautiful, showing the incredible profusion of connections within a developing brain.

Left: Multi-shell high angular resolution diffusion data decomposed into a free water component (greyscale background image) and a directionally resolved brain tissue component shown as rendered surfaces. Middle and right: Visualisation of anatomical connections in the developing brain derived from the brain tissue component.
MRI (or whatever you call these kinds of data maps, MRI seems much too simple a term) is an extremely important research tool, which is not the same as saying everyone should have an MRI!
Both term equivalent MRI and Ultrasound have very limited predictive ability for the former very preterm infant. This study shows, much more clearly than any before, that for an individual baby an MRI adds very little to an ultrasound, and that all former very preterm require health and developmental surveillance regardless of their imaging findings.