The Lancet just published back-to-back articles from the iCOMP collaborative reporting the results of the Individual Patient Data Meta-analysis of trials of differing cord management techniques in preterm infants. There were 48 trials with a total of 7000 patients in the IPD which made 3 comparisons Delayed compared to immediate clamping, and each approach compared to cord milking. Seidler AL, et al. Deferred cord clamping, cord milking, and immediate cord clamping at preterm birth: a systematic review and individual participant data meta-analysis. Lancet. 2023.
The data were analysed by subgroups above and below 32 weeks. Above 32 weeks there was very little evident impact on the outcomes that they analyzed, IVH, need for transfusion, NICU admission, and temperature on admission; which is what you would expect. The advantages in larger babies are probably more long term, with higher iron stores and less later anaemia.
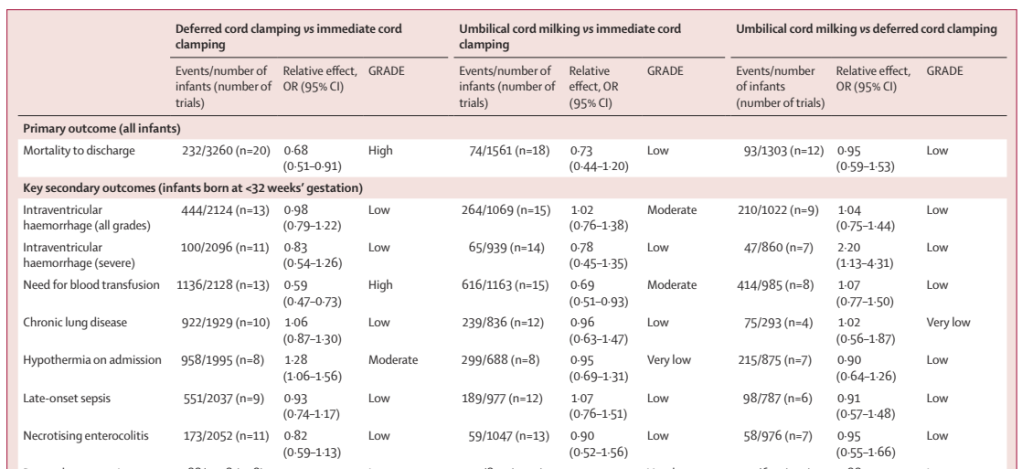
Below 32 weeks the results can be seen below: clear advantages of DCC compared to ICC; no major advantages of cord milking compared to ICC; and the major difference between DCC and milking being more severe IVH with cord milking.
For the first comparison, 80% of the weight of the meta-analysis of mortality comes from 3 trials, APTS 58%, a trial from Egypt which is inaccessible, (not listed on Pubmed, or in Embase, and the journal does not appear to have a website, so I am unsure how iCOMP even found it!), weight 14%, and the UK CORD pilot trial (8% weight). The remaining are all small trials with between 4 and 50 per group. The CORD pilot trial was a trial of at least 2 minutes of DCC, with resuscitation, if needed, with the cord intact.
Other analyses performed included the impact of multiple delivery (only available for 4 trials, many trials have excluded multiples) and of gestational age. Neither of these factors appear to have an impact on the advantages of DCC.
The second paper tries to evaluate the data regarding how long to delay cord clamping (Seidler AL, et al. Short, medium, and long deferral of umbilical cord clamping compared with umbilical cord milking and immediate clamping at preterm birth: a systematic review and network meta-analysis with individual participant data. Lancet. 2023), dividing the studies up into 3 groups, 15 to 45 seconds, 45 seconds to less than 120 seconds, and 120 seconds or more. Almost all of the information for the longest delayed group comes from the same UK CORD pilot trial, the other trials with longer delays had more predominantly mature infants, and therefore few events. In particular there were very few severe IVH, so they don’t even report that, in the UK trial there were 6 and 7 severe IVH in the two groups, and the other trials had tiny numbers of babies at risk, or excluded the most immature, or had 0 events.
The analysis of the longest duration of delay therefore relies almost entirely on the results of the CORD pilot trial, which was a well-done trial, delaying cord clamping for at least 2 minutes, and even longer if the physicians felt comfortable waiting for longer, up until there was no evident pulsation. Babies needing resuscitation were treated next to the mother on a hard surface. Many babies in the DCC group actually had clamping earlier as can be seen here:
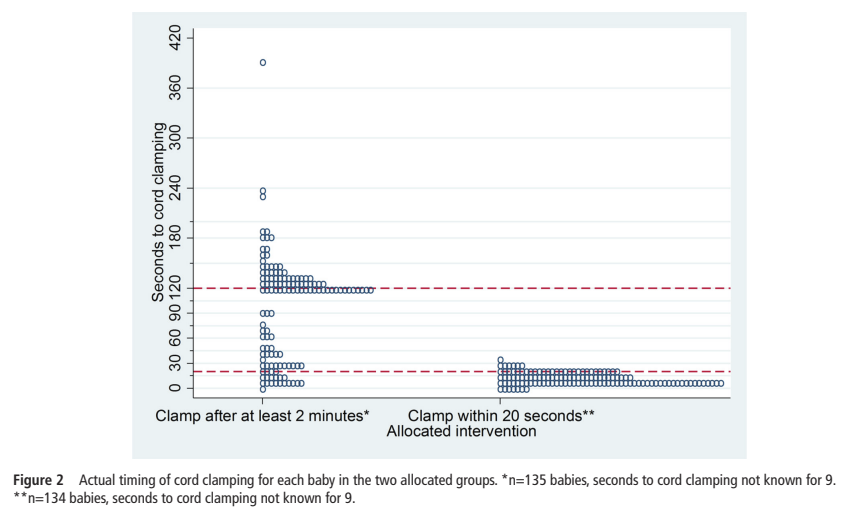
Many of the early clamped babies in the DCC group of the CORD pilot trial had good reason for early clamping, such as abruption, or the baby being born with the placenta, but many were because the “cord was too short” which, the authors note, became less frequent with time, or for “clinical decision”, which is not further explained.
I remain somewhat sceptical about Network Meta-Analyses, especially for indirect comparisons, where interventions that have not been directly compared are evaluated against each other as if they had been. The huge advantage of a true RCT, that all confounding variables tend to even out, those which you know about as well as those you don’t, is lost with an indirect comparison, such as in an NMA. No matter how much effort is put into correction for baseline imbalances, there always will remain the possibility of residual confounding.
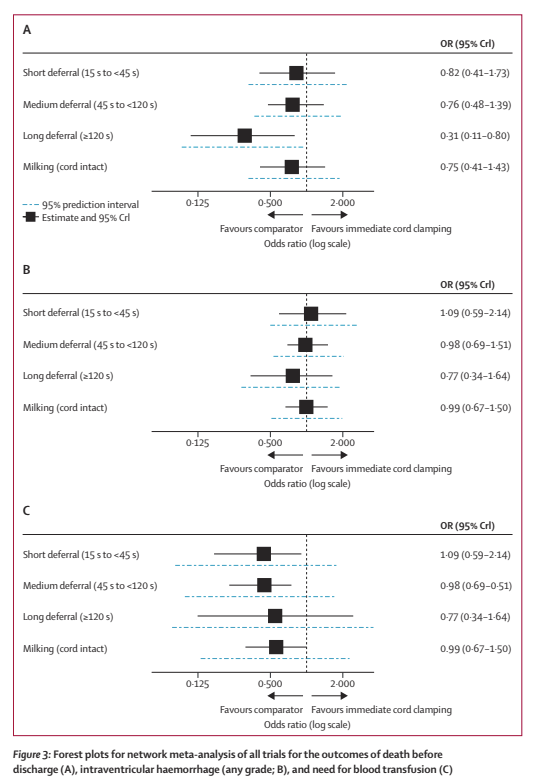
The results of the NMA for these 3 outcomes (all are compared to ICC as the reference group) suggest that the longest delay gives the most mortality benefit. But I don’t think that this should lead to everyone aiming for 2 minutes in every baby. Only one tiny trial directly compared short duration DCC to longer duration. But the NMA, showing the biggest reduction in mortality with the longer delay, is mostly dependent on the trial of Duley, which, individually, showed a small reduction in mortality with longer delay in clamping, which may have been due to random variability. Although this trial had more deaths in the ICC group, the difference in deaths was almost entirely among larger babies of 26 to 32 weeks (8/108 deaths compared to 1/107) and may have been a random occurrence in a smallish trial.
The NMA gives sufficient evidence that further trials examining the relative impacts of 60 to >120 seconds of DCC are warranted. The ABC3 trial was presented recently at the JENS meeting in Rome, it was a trial in very preterm infants comparing an approach similar to what many are currently doing, that is, immediate clamping if the baby needs intervention and DCC of 30 to 60 seconds if the baby is doing well. This approach was compared to DCC and clamping being performed after the baby was stabilised, with a good heart rate and oxygenation, resuscitation if needed was performed with the cord intact, and clamping could be delayed up to 10 minutes. There were no differences in the outcomes reported at presentation of the results, mortality or IVH. I think we should therefore wait until this, and other ongoing trials are published, before longer delays in clamping, and resuscitation with an intact cord becomes the standard.
Take home messages: for mildly preterm infants at low risk of IVH, DCC is preferable to ICC, but milking may be a reasonable option if DCC is not feasible; for very preterm infants at risk of mortality or IVH, DCC is preferable to either ICC or milking. Longer durations of DCC, with resuscitation on an intact umbilical circulation, are not yet proven to further improve mortality or other clinically important outcomes.









One thing that is often forgotten is that early cord clamping was not based on any evidence that it was better. It was just chosen as part of the active management of labour to try and reduce pph.
Another thing to remember is that in nature, farming, veterinary practice, the cord is not cut early and is left alone.
I don’t like the idea that the cord is cut/ligated at a set time after birth. That is not based on any good data. If we want guidelines then wait until the baby has established breathing and curd pulsation has stopped