Two new publications, in the Journal of Pediatrics, report trends in definitive closure of the PDA. This is a subject that I haven’t written about much on the blog, I wrote about the Beneductus trial last year, which was an RCT of early ibuprofen treatment of large PDA between 24 and 72 hours of age, compared to expectant management, without cox inhibitors, but with eventual surgical closure if needed. But I haven’t posted often about the PDA, and never, I think, about surgical/catheter closure.
You can see from the CNN 2021 report that there has been a dramatic reduction in definitive closure of the PDA (with surgery or a “device”) across Canada over the previous 11 years.

I guess for me the subject is murky, but as far as I can see through the murk, there is no clear indication for closing any PDA in the preterm. Outcomes between active treatment approaches and very restrictive approaches are quite similar. There is a very recent systematic review (Cheema HA, et al. Expectant management of patent ductus arteriosus for preterm infants: a meta-analysis of randomized controlled trials. Am Heart J. 2023) that examined clinical outcomes in trials which compared active therapy to trying to leave the PDA alone. They arbitrarily decided to include only trials with <25% rate of active treatment in the control group, I don’t know why 25% was the magic number. They showed no benefit of active treatment on mortality (all cause) or NEC, these 2 Forest plots are of mortality, and then NEC. (The figures are copied from the pre-proof, hence the watermark, or from the on-line supplement).


They found 7 trials that fit their criteria, 4 of them had very low rates of treatment among controls, between 0.7% (the Beneductus trial) and 8%. One of the trials was an RCT of prophylactic indomethacin, without confirmation of the presence of a PDA, so it was not an RCT of different approaches to the PDA.They also (Nair 2004) did not report the rate of treatment in controls, and it should really not have been included in this SR. Van Overmeire’s trial had a 24.8% rate of control treatment with cox inhibitors.
The review shows an increase in BPD with active treatment, as this Forest plot shows

The 95% confidence intervals cross the line of no difference, however, and if you delete the trial from Nair, with unknown control treatment rate, and unknown PDA status at the start of the trial, and Van Overmeire, with 25% treatment of the controls, then there is probably not likely to be a major impact on BPD one way or the other, but it seems that there is unlikely to be an improvement in BPD.
The following data from Pediatrix, (Shah ZS, et al. Trends in Procedural Closure of the Patent Ductus Arteriosus among Infants Born at 22 to 30 Weeks’ Gestation. J Pediatr. 2023:113716) among babies of <30 weeks gestation show a similar trend to the CNN, and they show the proportion with device closure, which has become more frequent than surgery. In the CNN, babies between 27 to 29 weeks now have an overall incidence of definitive closure of <1%, so a similar rate of definitive closure, and a major change in clinical practice over 10 years or less.

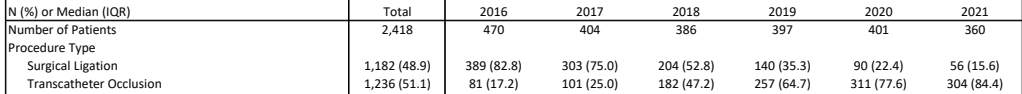
The other publication is from the Children’s Hospital Association in the USA, (Lai KC, et al. Current Trends in Invasive Closure of Patent Ductus Arteriosus in Very Low Birth Weight Infants in US Children’s Hospitals, 2016-2021. J Pediatr. 2023:113712) and only includes very preterm babies (<32 weeks) who were admitted for definitive PDA closure to a children’s hospital that was submitting data, between 2016 and 2021. The first surprise to me in this paper is that the number of admitted babies was relatively stable. I wonder where they are all coming from! As you can see from the part of the table that I reproduce below, apart from 2016, the numbers haven’t been going down very much, compared to the 2 other sources of data I have discussed. Of course, the ascertainment is completely different, but I would have expected a bigger drop in overall numbers, maybe referral patterns have changed.
They do, however, note the dramatic shift from surgery to catheter occlusion. They also note that the catheter procedures are being performed progressively earlier, decreasing from a median of 38 weeks PMA to about 31 weeks, and now similar to the age of surgery.
This dramatic change has taken place without any robust evidence that catheter occlusion is preferable to surgery. Or even much data that it is equivalent. I understand the desire to avoid a thoracotomy, but what is the relative impact of the 2 approaches on clinical outcomes? What is the relative effect on vocal cord paralysis and on vascular compromise? I presume that vocal cord paralysis would be much less frequent with catheter closure, and that vascular compromise of the limb that was used for the catheter would be much more common, but this incredible shift in practice, that has occurred without good studies, is worrying. The meta-analysis that was published a couple of years ago included only observational studies, there were no RCTs included comparing catheter closure to surgery. Its interesting also that the prominent, non-randomized trial of the Amplatzer device (Sathanandam SK, et al. Amplatzer Piccolo Occluder clinical trial for percutaneous closure of the patent ductus arteriosus in patients >/=700 grams. Catheter Cardiovasc Interv. 2020;96(6):1266-76) has the longest list of conflicts of interest that I can remember in neonatology:
S. Sathanandam: proctor/consultant Abbott; D. Gutfinger: full‐time employee Abbott; L. O’Brien: full‐time Abbott employee; T. Forbes: proctor/consultant Abbott, Edwards, AcuNav/Biosence Webster, B. Braun Medical, Siemens, Medtronic; M. Gillespie: proctor/consultant Abbott; D. Berman: proctor/consultant Abbott, Edwards, Medtronic; A. Armstrong: proctor/consultant Abbott, Edwards, Medtronic, B. Braun; S. Shahanavaz: proctor Abbott, Medtronic, and Edwards; T. Jones: research grant, proctor/consultant Abbott, Edwards, Medtronic, W.L. Gore & Assoc.; B. Morray: Consultant Medtronic, proctor Abbott; T. Rockefeller: proctor Abbott; H. Justino: proctor/consultant Abbott, Edwards Lifesciences, Medtronic; Clinical trial executive committee Janssen Pharmaceutical; Co‐founder PolyVascular; scientific advisory board Pediastent; D. Nykanen: proctor Abbott, consultant and independent data reviewer W.L. Gore & Assoc, expert witness Glaxo Smith Kline; E. Zahn: consultant/proctor Abbott, Edwards, Medtronic, National PI ADO II AS IDE Trial and Alterra/S3.
The 2 new publications give some data about outcomes: in the Children’s Hospital Association study the incidence of reported arterial thrombosis in the surgical closure group was 1.6% and venous thrombosis was 6%, with 3.6% being anticoagulated after the procedure. In the catheter occlusion group the arterial thrombosis incidence was 3.6%, and 4.4% had venous thrombosis, with 4.8% receiving enoxaparin. As the data are from an administrative database it isn’t clear if the thromboses occurred before or after the procedure, I presume they are retrieved from the recorded list of diagnoses during the hospitalisation. With the same limitations (and without necessarily routine surveillance) vocal cord paralysis was recorded in 4.8% of the surgical and 0.5% of the catheter closure group. There was less opioid use post-op in the catheter group (52% vs 87%).
The Pediatrix group study shows similar mortality in the surgery group to the catheter closure group, and a slightly shorter length of hospital stay (103 vs 109 days). It is hard to know what to make of length of stay in the other study, as many babies were transferred back to their hospital of origin.
I remain uncertain about the indications for definitive closure of the PDA. Most babies, even with a persistent shunt, can be weaned from respiratory support, and sent home, and most will eventually close spontaneously, although you might have to wait a few years. (Nielsen MR, et al. The chance of spontaneous patent ductus arteriosus closure in preterm infants born before 32 weeks of gestation is high and continues to increase until 5 years of follow-up. Acta Paediatr. 2022;111(12):2322-30). If you do need definitive closure, catheter occlusion looks like a reasonable alternative, and may be preferable, but it would be nice to have better data to confirm that.









As being quite a novice I was thrilled with the outcomes of this study:
https://www.sciencedirect.com/science/article/abs/pii/S014600052300023X
A more of a precision medicine approach. We’ll see if it’s replicable, but the results are very favourable. The beneductus trial didn’t really evaluate the actual hemodynamic compromise of the duct as I understand it, thus somewhat missing the target.