Recommendations for older children and adults during endotracheal intubation frequently include the use of free flow oxygen, indeed when I was a fellow with Neil Finer we routinely provided additional free flow oxygen from a catheter placed near the nose, a practice based on data from older subjects. As practices changed with the introduction of routine premedication I didn’t continue the practice, reasoning that intubation with premeds was a lot faster, and that the babies were not breathing anyway. This was probably a mistake. Apnoeic oxygenation is something that is well described in various situations, and I have used it to prevent desaturation during apnoea tests for brain death in the PICU. At the same time the development of readily available high-flow nasal cannulae makes provision of a free gas flow during intubation easier, and probably more effective than just holding an oxygen tube near the baby’s nose.
Studies in adults and older kids have shown that having high-flow cannulae in place during intubation delays desaturation, which is a very common reason for terminating an intubation attempt, and leads to reduction in the number of attempts prior to successful intubation.
Not surprisingly it is the Melbourne group who have taken this to a clinical trial in newborn infants. (Hodgson KA, et al. Nasal High-Flow Therapy during Neonatal Endotracheal Intubation. N Engl J Med. 2022;386(17):1627-37), the Stabilisation with Highflow for Intubation of NEonates, SHINE trial. They randomized 251 intubations (in 202 infants) to either have high-flow nasal cannulae (HFNC) placed prior to intubation, or not. Babies of all gestational ages were eligible, and intubations in the delivery room or the NICU were included, if the intubation was not an emergency.
HFNC were used at a flow rate of 8 litres for all the infants, and used the same oxygen concentration that the baby was already receiving, with the opportunity to increase to 100% if the SpO2 fell below 90%. The primary outcome variable was success on the first attempt, without instability, which was defined as hypoxia (>20% decrease in SpO2) or bradycardia (<100 bpm). Three quarters of the intubations were in the NICU, and most were pre-medicated, with the same protocol that we use in my centre, and which is recommended in several guidelines, atropine, succinylcholine and fentanyl.
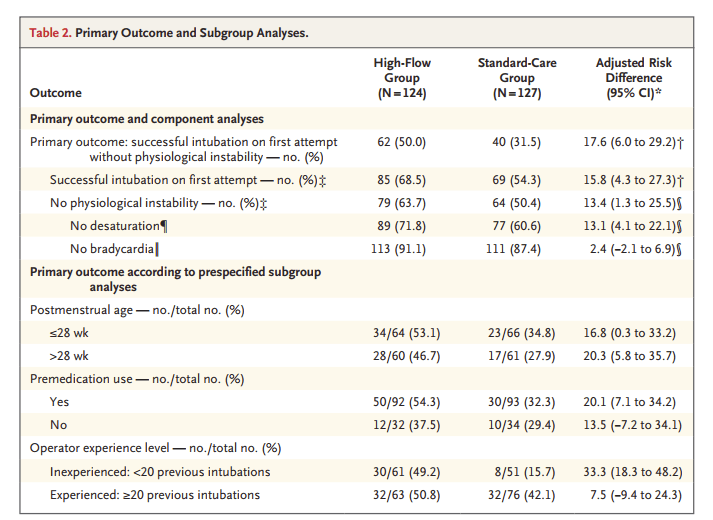
As you can see from the primary outcomes, there was a much higher rate of success on first attempt without desaturation or bradycardia, which appears to be mostly because of less desaturation, and there was not any significant occurrence of hyperoxia. You can also see that the biggest gain was among those with less experience, with a dramatic improvement in success, but there is probably an improvement among those with more experience also.
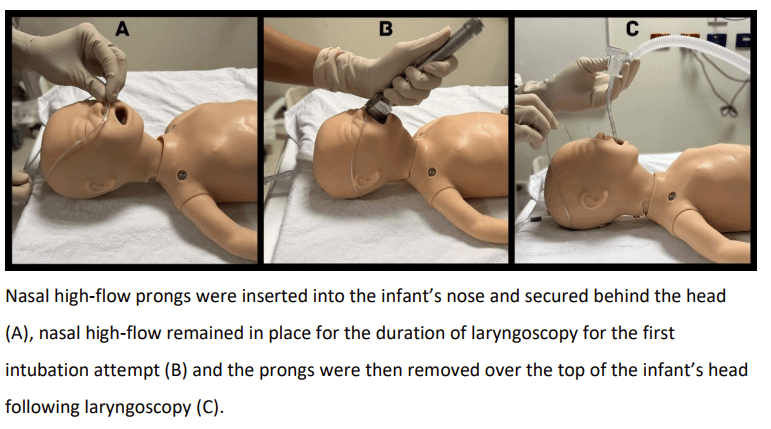
If you have access to the NEJM you can watch a video of a real-life intubation with HFNC, but it really is quite simple, as the image below shows.
There doesn’t to me seem to be any good reason to not implement this widely. There were unfortunately few intubations with a video laryngoscope (only about 8%), which other data show improve success, especially with inexperienced operators. But the two approaches are not in any way exclusive, using HFNC and a video laryngoscope might be the best possible approach, especially for inexperienced intubators, which is now the majority of paediatric trainees! Now that we intubate very few meconium stained babies, we try to maintain as many babies as possible on non-invasive ventilation, and we have a tiny baby intubation team, there are few opportunities for trainees to intubate real babies. Simulation training is vital in providing initial training, but making intubation safer for real babies when it becomes necessary, and ensuring that paediatricians in training develop the expertise needed are all important.
This new publication, and the technique that it shows is safe, effective, and simple, is a big advance for neonatal intensive care.









Does the flow need to be heated and humidified when the median duration of procedure is about 50 seconds?
That may help lower costs and time to set up, which is a significant consideration in most units.
I think that for larger babies high flow unheated dry gases would probably be OK for a short time, maybe more of a problem for the tinies, and especially if it goes on too long.
In the UK, most places using delivery room CPAP use unheated dry gases until they are admitted to NNU, which is usually >15 minutes. Although admittedly, most of these babies are over 26 weeks.
Any reason we can’t leave them on CPAP during intubation? That’s what we do for MIST/LISA?
It would probably work, it might be a question of practicality, depending on what sort of interface the baby has, it could really get in the way. The HFNC are very low profile.
My understanding of this paper was that Using HHFNC @8lpm provided a distending pressure and also filled the nasopharynx with oxygen which may have contributed to reduced desats.
Isn’t this approach different to NRP about holding free flow oxygen during intubation.
I never understood the mechanism behind apnoeic oxygenation in neonates with free flow oxygen wafted around external nares helps in oxygenation in apnoeic infants.
Hi Keith, very good trial. I do not understand the reason for using 8 l/min universally. It is a super flow rate for tiny babies. What are your thoughts? Thanks!
Our team has reviewed that article recently. I agree with Dr. Barrington and the authors that it is of greater interest to less experienced operators, who are a majority in many neonatal units. But 90% of the patients in this series were previously on CPAP. With our experience in the LISA/MIST method, in which children tolerate the procedure better, we currently do not wean the patient from CPAP during intubation. But we see it as very interesting for those babies who are intubated in the delivery room without extreme urgency, or in the NICU without prior respiratory support. The main technical difficulty that we find is in some situations where it is necessary to have 3 respiratory support systems working at the same time, with their corresponding oxygen and air intakes. As can be seen in the NEJM video, a mask-IPPV system (or CPAP/NIV), the HFFNC system, and a ventilator would be required working simultaneously. In some environments it can be difficult to have so many resources available. That said, we agree with Dr. Barrington, this is a step forward that we will need to implement in all neonatal units.
Hi Keith,
Interesting article!
Do you think that using RAM cannula and delivering CPAP through it in preterm infants would be a better alternative to HFNC to minimize desaturations before intubation or surfactant delivery? Thanks
The RAM cannulae are very problematic as they have such a high resistance, that very little CPAP is actually delivered to the baby. You also have the same problem as with HFNC, that the nasal leak is variable. WIth HFNC at 8 lpm you can get high CPAP or very little CPAP, I don’t think you can extrapolate to other systems directly, but having a continuous flow of a gas mixture during the entire intubation process is probably key here, rather than the variable positive pressure provided. I think with the mouth held wide open by a laryngoscope you probably don’t have much positive pressure during the laryngoscopy phase, so it is probably the gas flow which is important.
Pingback: Making intubation safer for the most fragile babies | Neonatal Research