It has been dogma for quite some time that newborn preterm infants with Inguinal Hernias (I will resist the temptation to latinise the plural, although I was brought up hearing about ‘herniae’) should have them surgically fixed prior to discharge home because the risks of incarceration were so much higher in the young infant.
This practice has been widely followed wherever I have worked; discharge has sometimes been delayed, depending on logistics and clinical status of the baby, and just about all of them have been surgically repaired prior to going home.
Anesthesia and surgery are not without risks, and the preterm infant at risk for such hernias is also at risk of cardiorespiratory instability during and after hernia repair. Delaying surgery might allow a more stable clinical status of the infant, if it can be safely done without increasing complications, in particular incarceration, with its risks of strangulation and intestinal obstruction.
This pivotal multicentre RCT was performed to answer the practical question “is repairing an Inguinal Hernia in a former preterm infant safer if it is performed before discharge home from the NICU, or if done post-discharge at more than 55 weeks PMA?”(HIP Trial Investigators. Effect of Early vs Late Inguinal Hernia Repair on Serious Adverse Event Rates in Preterm Infants: A Randomized Clinical Trial. JAMA. 2024;331(12):1035-44)
So the primary outcome was “safety” which was defined as the absence of any serious adverse event. These “included pulmonary events (apnea requiring intervention, prolonged intubation, unplanned reintubation, stridor, pneumonia), cardiac events (bradycardia requiring intervention, cardiopulmonary resuscitation, cardiac arrest), surgical events (intraoperative injury, wound disruption, surgical site infection), events related to the hernia (incarceration, recurrence, reoperation), and death”. Babies were eligible if born preterm (<37 weeks) and had an Inguinal Hernia. They were enrolled and randomized when thought to be 2 weeks from being discharged.
Clearly some of those outcomes are much more important than others, and this is one issue that we could have with the trial. If there had been more deaths in one group, but more apneas in the other group, then the overall number of SAEs might be identical, but clearly one outcome is worse than the other! Indeed, the main real difference in outcomes was many more apneas in the early repair group.
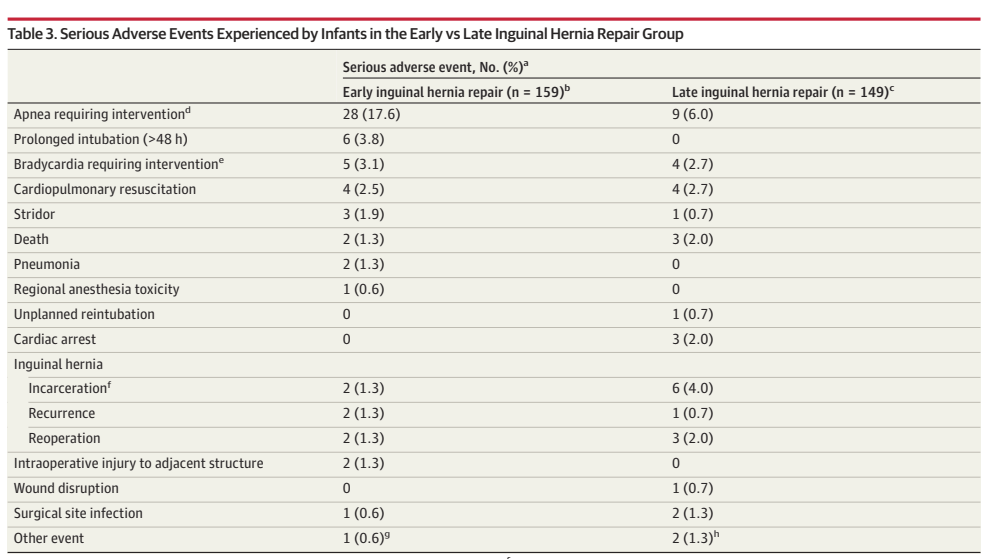
There was, overall, at least one adverse event in 28% of the early and 18% of the late group.
As you can see, all the other components of the primary outcome were uncommon, including, most importantly, incarceration, for which the absolute risk difference was 2.7%.
One other outcome of interest were the reasons for non-repair in the 2 groups, among the early repair group, 7 had the hernia resolve spontaneously between enrolment into the trial and the date for the surgery. In the late group 17 babies had resolution of their hernia. I think this is a major advantage of delaying surgery, another 8% of the infants will never need to have the surgery if it is delayed!
As a practical trial, there were many babies who had early repair despite being in the late group,

including due to parent or clinician preference (one could argue that such babies should not have been randomized) and 11 because “concerned about incarceration”, which isn’t really explained, does that mean that there were some signs of incarceration? or someone was just worried?
The analysis was Bayesian, so the results are presented as the likelihood that late repair is preferable to early repair, in terms of numbers of adverse events. For the group as a whole, using a neutral prior (meaning there was no previous good evidence that one approach led to fewer SAEs than the other) the posterior probability of an advantage of the late group was 97%. On subgroup analysis, the major difference in SAEs was among the more immature babies (more than 99% probability of benefit of delaying), compared to 28 weeks GA or more; and among those with BPD.
This is presumably because it is the very immature baby who has a major risk of peri-operative apneas, babies over 28 weeks rarely have such events, so will not have much of that particular benefit, which was the only large difference between groups. The other large benefit of late repair, in relative terms, was avoidance of prolonged assisted ventilation post-op, this occurred in 6 early and 0 late repaired babies, which is presumably related to why late repair was more beneficial in babies with BPD than those without.
I think this trial should have an immediate impact on practice. If safe surveillance can be ensured, then infants at high risk of perioperative apnea, that is, those <28 weeks, have a benefit from late repair, after 55 weeks. Where I live and work, some families come from hundreds, or even thousands of kilometers away, and may have difficulty being transferred back for surgery, especially if it is urgent; they could continue to have pre-discharge repair, because the major increase in risk is for apnea, which is a short-term complication that we can monitor for.
For those who live on or close to the island of Montreal, they can be discharged a little earlier (mean of 5 days sooner in this trial) and the hospitalisation for the hernia repair is usually very brief (mean 0.5 days).
As a more theoretical, study design, consideration, future trials should construct ordinal outcomes, which take into account the relative importance of the outcome variables. As it happens, in this trial I think the relative rarity of all outcomes other than apnea, and the lack of any big difference between groups, means that a DOOR type analysis would almost certainly have given the same results.









Journal club sur le sujet le 19 novembre à 14h?
Keith, could you present it? Or we could as our fellows or surgical fellows?
Annie
Hi Keith, thanks for this. In Ottawa, we reviewed this article a few months ago with our surgery colleagues and agreed to proceed with a delayed repair when safe (not living too far).
In our current practice at at a level 3 nicu in los angeles, we have moved to delayed repairs. I however still wonder about the need for general anesthesia, when there are studies that suggest that regional anesthesia may be better. It is akin to still doing C sections with general anesthesia in my humble opinion. Regional anesthesia link