For those who are unaware, the Silverman Lecture is an annual honour bestowed by the AAP. A neonatologist who has made. or is making, major impacts in neonatology is asked to deliver the lecture. Bill Silverman was one of the early pioneers of neonatology in the USA, and was very outspoken about the need for evidence-based practice (having performed some of the earliest RCTs in neonatal medicine himself).
This years lecturer was Annie Janvier, and, for the first time ever, a second speaker was invited to collaborate on the presentation, a mother that Annie (and I) have worked closely with, Rebecca Pearce. Rebecca and Annie have both had extremely preterm infants, Rebecca recounted, at the start of her part of her talk, that she had twins Lily and Maren at 25 weeks. Lily died within her first few days of life of early onset septicaemia, and Maren, who also had EOS, survived. Rebecca and her husband have written about their experiences with the pre-discharge MRI, and they have become valuable members of our parent resource team at Sainte Justine. One particularly moving part of her presentation was a slide which listed on one side all of the diagnoses that Maren has had from doctors (including various delays and executive function disability), in the middle was a picture of a lovely smiling 14 year old girl, and on the other side a list of her characteristics as seen by her family, “caring”, “warm”, “bubbly” “hard worker”.
Annie’s presentation recounted, a little, our course with Violette, including this briefly shown picture of me doing kangaroo care in the NICU!

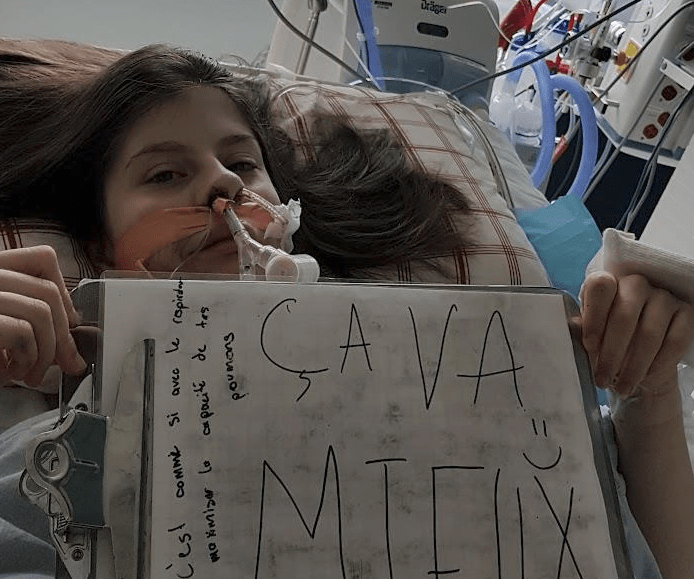
It also included pictures of Violette in the PICU, intubated after her tracheal reconstruction at the age of 15. She noted that Violette did not have “BPD”, as she came out of oxygen a couple of days before she hit 36 weeks, but that she certainly had respiratory fragility, and had serious upper airway problems, receiving several courses of steroids for stridor with signs of obstruction during her first few years of life. An outcome which has rarely or never been described in neonatal follow up studies, but which is well known to paediatric ENT surgeons. (As you can see, the image is from a day or two after the surgery when “ça va mieux”, things are going better).
Annie described the work of the “Parents’ Voices” project, which was created to “Engage Parents to Co-create” definitions of what are important outcomes of neonatal care, on which Rebecca is a co-investigator .
One of Annie’s slides, which illustrates that our current measures of “NDI” don’t reflect what parents think about their children, was derived from data in one of the Parents’ Voices publications. It showed that, when we categorize infants as having No NDI, mild-moderate NDI, or severe NDI, parents often disagree with us, a disagreement that increases the more “impaired” we think their child is. Only 12% of parents whose child was categorized as sNDI agreed that their child was severely impaired, a third of parents of such children don’t find them impaired at all. On the other hand there were 25 parents who found their child severely disabled, 22 of them were classified sNDI by the CNN definition, but 3 had either no or mild NDI.
Annie listed some of the publications from the project to date (and there are more to come!):
As you can see I am co-author on some of them, being a collaborator, rather than a member of the core group. I am proud to be associated with this group who are making great strides in re-defining what outcomes are of importance to families. The CNFUN is incorporating many of the measures that parents find important, for which validated instruments exist, into the national follow up database.
Here are the 2 Silverman Lecturers on the big day:

The lecture was greeted with a standing ovation from the audience,
This was followed by a Q&A session, which was generally thoughtful and appreciative. Unfortunately it ended with a comment from a retired neonatologist who said two things: Firstly, that quality of life is subjective, so shouldn’t be used as a primary outcome. I’m not sure I agree, you can measure quality of life just as well as you can measure the incredible complexity of child development; the person posing the question led a few very high quality studies (2 of which I was involved in), in which, unfortunately, like so many others, we dichotomised the richness of children’s developmental progress into “pass” or “fail”, “NDI or “no NDI”. I would agree, however, that you shouldn’t divide quality of life into 2 categories, of good or bad QoL. But in a sense, unless an intervention improves some aspect of QoL then what value is it? Secondly, they also stated that it is important that there is link of scientific plausibility between the intervention and the outcome. That is self-evident, and indeed what the Parents’ Voice project is trying to do is to develop more appropriate plausible outcomes: Parent-Important respiratory outcomes for respiratory interventions, Parent-Important developmental and neurological concerns for Neuroprotection studies.
The outcomes that are important to parents are also, often, the outcomes that are important to society as a whole, and that often have an impact on medical resource use. To take an example from the previous post, it matters little to anybody if a baby needs a few more days of oxygen while they are hospitalised. What matters to parents, and has an impact on society and resource use, is if discharge is delayed by pulmonary concerns (such as oxygen dependence), or if the baby needs oxygen at home, or has recurrent admissions post-initial discharge, or has difficulty feeding because of tachypnoea, etc. Until we start to measure such things, we have little idea if our interventions are having an impact on outcomes that really matter.









Good morning, Keith,
You must have misunderstood my comment about the outcome “quality of life”.
I did not say that this outcome can’t be measured! However, I did say that quality of life should not be the PRIMARY outcome in a clinical intervention trial because this outcome is subjective. But I added that quality of life can be an important SECONDARY outcome in a randomized trial.
Since you were involved in the CAP trial, you may remember that we measured self-reported quality of life in the CAP trial participants when they were 11 years old:
Self-reported Quality of Life at Middle School Age in Survivors of Very Preterm Birth: Results From the Caffeine for Apnea of Prematurity Trial.
Schmidt B, Anderson PJ, Asztalos EV, Doyle LW, Grunau RE, Moddemann D, Roberts RS.JAMA Pediatr. 2019 May 1;173(5):487-489.
I apologize for misquoting you, I will change the post.
Keith
Keith: You wrote this “One of Annie’s slides, which illustrates that our current measures of “NDI” don’t reflect what parents think about their children, was derived from data in one of the Parents’ Voices publications”
Could you post the slide or the reference?
Thanks,
Alfonso Pantoja, MD
The slide is from a publication which is undergoing peer review at present, so Annie asked me not to post the actual figure. I will highlight it when it is published. There are also similar data from another of the Parent Voices publications This one :Synnes A, et al Redefining Neurodevelopmental Impairment: Perspectives of Very Preterm Birth Stakeholders. Children (Basel). 2023;10(5).