In addition to the short term results that I just posted about, the publication from the NICHD NRN describes the longer term outcomes of the babies of 22 to 26 weeks GA born between 2013-2016 who completed their 2 year follow up.
I was pleased to see a detailed summary of multiple different outcomes, despite the persistence of “NDI” as an outcome and its division into “severe NDI” defined by any of a Bayley-III cognitive composite score or motor composite score less than 70, GMFCS level 4 or 5, bilateral blindness, or severe hearing impairment, and “moderate NDI”, defined as any of a Bayley-III cognitive composite score or motor composite score of 70 to 84 or GMFCS level 2 or 3.
At the risk of boring my readers, I will quickly re-iterate why I am opposed to using this terminology, and these definitions, you can skip the next 2 paragraphs if you are already in agreement with me! An impairment is defined by the CDC as “an absence of or significant difference in a person’s body structure or function or mental functioning”, the WHO definition is “problems in body function or structure such as a significant deviation or loss”. A low score on a developmental screening test does not satisfy either of these similar definitions. Cerebral palsy of sufficient severity to impact function can be considered an impairment, hearing and visual losses also, but a low score on the Bayley Scales of Infant Development (BSID) is rather different. Most infants with low BSID scores will not have similarly low scores when intellectual abilities are measured later, whichever version of the BSID you are referring to, and whichever threshold you pick. As most infants categorized as “impaired” fall into that category because of low BSID scores, this is an important consideration. It would be better to call this Neurologic Impairment or Developmental Delay, to emphasize that, for a substantial proportion of infants with low BSID scores, it is indeed a delay in development, rather than a “cognitive impairment” which is a term often used to describe low BSID scores. Also, importantly, “severe NDI” is often used as shorthand for “handicap so severe that it makes neonatal intensive care futile” and is then often often conflated with death as an outcome which no-one would really want, and used for counselling parents.
Additionally, these categories have been created by physicians, with little input from families. Do parents agree with our categorization? Certainly, some do not, (Janvier A, et al. Measuring and communicating meaningful outcomes in neonatology: A family perspective. Semin Perinatol. 2016;40(8):571-7), which is an article Annie and I wrote with 3 other parents who had experience of a baby in the NICU. An ongoing project is examining how parents describe the outcomes of their infants, and has found little agreement between parental evaluations and NDI categories. (Jaworski M, et al. Parental perspective on important health outcomes of extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2021:fetalneonatal-2021-322711). I certainly don’t think that, if you asked a parent about what happened to their infant, born extremely prematurely, they would be likely to respond, “they are either dead or blind or have slow development”.
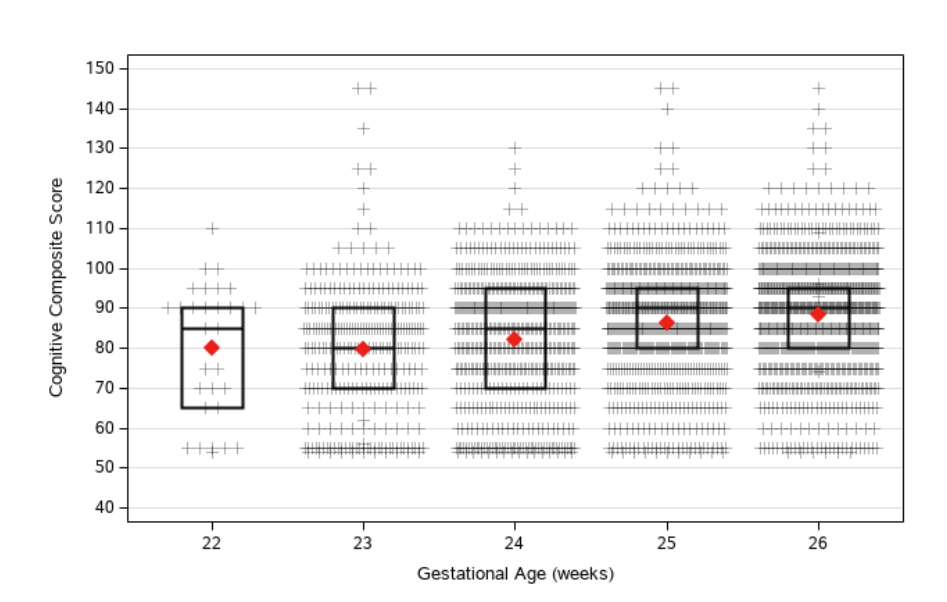
Thankfully, this publication has a much more detailed description of outcomes of the babies between 22 and 26 weeks gestation, which is much more useful than just categorizing them into one of 3 arbitrary groups. In the supplement are these very informative figures for each of the BSID scores:
The BSID scores are also described in this table, which give the scores on the 3 composites, with the means, medians and numbers below certain thresholds, by gestational age and overall:

The graphs and table show that the median BSID scores do not vary that much by GA, but there is a higher proportion with low and very low scores on each of the 3 scales at 22 and 23 weeks. This much richer summary of outcomes is much more informative that simplistic categorizations, and should be standard.
The GMFCS outcomes (gross motor functional classification scale, a way of grading cerebral palsy) from the same table, with the same order of columns, show substantially more cerebral palsy of moderate and severe degree as GA decreases.

Another thing that I really appreciated about this publication is the lower part of the table, which includes many things that are not often reported;
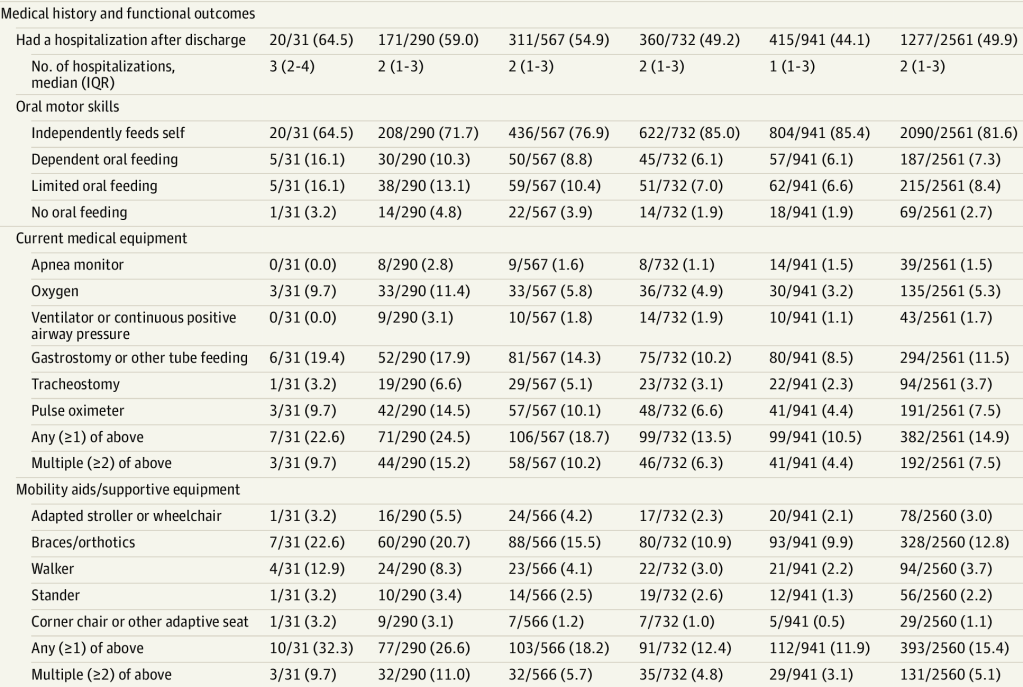
Hospitalisations, feeding competence, and medical equipment at home are all things that have a big impact on families, but are usually not reported. Most babies at all GA had some oral feeding at follow-up, but the most immature babies are much more likely to have limitations in feeding skills. Additionally mobility aids are more frequently required, which goes along with more frequently having a GMFCS indicating significant CP, and more frequently having BSID motor scores below thresholds. As for re-hospitalisation, more than 50% of them were for respiratory indications (data in the supplement) followed by surgeries, other infections, and then a variety of other indications, including 5% for growth and nutritional issues.
There is no information presented here about behavioural or emotional issues, even though they are of importance to families, but at 2 years of corrected age I can understand the difficulties in analysing them. It is impossible to tell from these presentations which infants had multiple problems; an infant with severe CP, blindness, major feeding problems and low BSID cognitive score, has a very different life course to 4 children with each of those problems individually. NDI categorizations don’t help with that either, as having any one of the supposed impairments qualifies the baby for the category, as would having multiple problems. In the future it would be helpful to have a summary of how many infants have 2 or 3 or more problems.
There is also no analysis of which risk factors are associated with more problems at follow up, probably there will be many more publications addressing those issues, but I can already predict that PVL and severe IVH are associated with worse motor function, that surgical NEC is associated with worse motor and cognitive scores, that late-onset sepsis is associated with poorer cognitive scores, and that BPD, especially if treated with steroids is associated with lower cognitive, language and motor scores. Preventing all of these complications will improve survival and will also improve long term outcomes.








