This is a very interesting trial evaluating the usefulness of clinical assessment of the circulation in adults with septic shock in a large international multicentre trial. Patients with suspected sepsis, who required norepinephrine after 1 litre fluid bolus, and had an elevated serum lactate, were randomized. A standardized method of measuring capillary refill time was agreed upon,
CRT was assessed by applying firm pressure to the ventral surface of the distal phalanx of a finger, using a glass microscope slide. The pressure was increased until the skin was blank, maintained for 10 seconds, and then released. The time required to return to the normal skin color was measured with a chronometer and a refill time longer than 3 seconds was defined as abnormal
and the algorithms were activated if the cap filling time was abnormal in the CRT-PHR (cap refill time- personalized haemodynamic resuscitation) group.
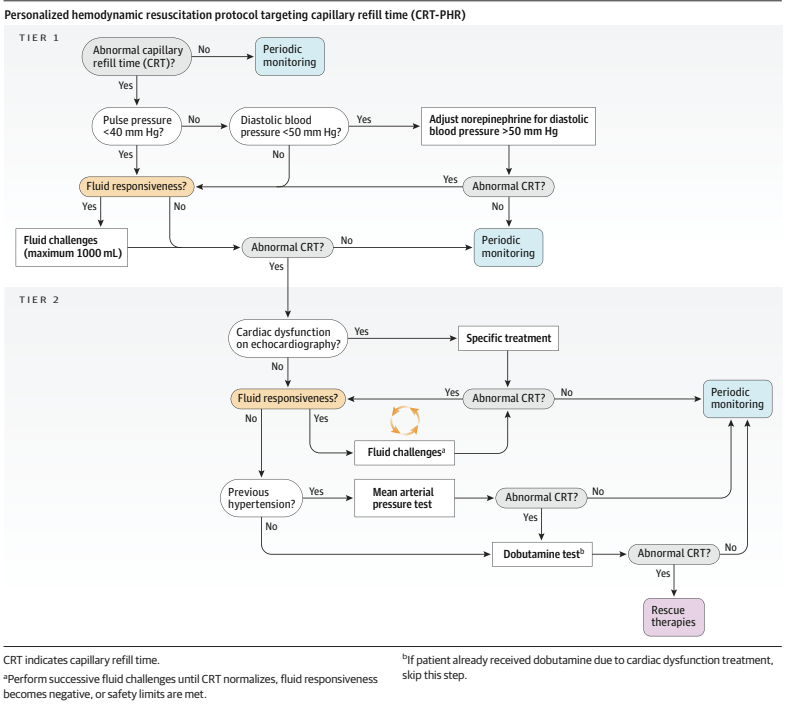
As you can see, if the CRT was >3 seconds, you first check the pulse pressure, and if it is >40 mmHg, then you check the diastolic BP, which may lead to increasing norepinephrine dose; the next stage may be to give more fluid to see if there is a response, and then progress to bedside echocardiography, which may lead to specific treatments, or more fluid, or eventually to low dose dobutamine.
The control group had “standard care”, CRT was recorded but the algorithm was not followed.
The primary outcome was a hierarchical composite: (1) all-cause mortality within 28 days, (2) duration of vital support (vasoactives, mechanical ventilation, and kidney replacement therapy) truncated at day 28, and (3) length of hospital stay truncated at day 28.
The trial was analyzed by the Win Ratio. 1400 patients were randomized, as it was not a paired study (one way of using the Win Ratio), but individually randomized, they stratified the patients by APACHE score, then, within strata, every patient in group 1 was compared with every patient in group 2, to determine if they won or lost. There were therefore 244 000 paired comparisons. The CRT-PHR group won 49% of the comparisons, compared to 42% of the control, usual care group. The remaining 9% were exact ties.
This exceeded the limits for statistical significance; mortality was identical at 26.5%, but there were more ICU free days, and shorter hospital stays in the CRT group. The table of interventions shows that more of the CRT group received vasopressin, more received dobutamine, and they received less fluid; at 6 hours of treatment, their CRT was shorter, and serum lactate was lower.
The analysis is illustrated below in the 2 strata of the Apache Score (a higher score predicting higher mortality); this showed a greater difference in the sicker patients.

I found this fascinating. In terms of the intervention being investigated, trial design, and analysis methodology.
Many of my readers will know of my concerns about the way we analyse composite outcomes in neonatology. Comparing “death or BPD”, “death or NDI”, “death or hiccups”, between randomized groups, as if they were of equal importance, and as if we were always sure that they would change in the same direction with an intervention. This trial is one of a growing trend to using hierarchical composites, with death being given the greatest weight in the analysis, followed by other clinical outcomes in descending order of importance. Clearly an example to be followed in neonatology.
As for the intervention, I remember from my years as a staff in the PICU that one of the best predictors of a good outcome after major cardiac surgery is that the nurse tells you the infant’s toes are warm! It is a better predictor of survival than measuring cardiac output, for example. (Here is a recent example Cruz G, et al. Capillary Refill Time and Serum Lactate as Predictors of Mortality and Postoperative Extracorporeal Membrane Oxygenation Requirement in Congenital Heart Surgery. Children (Basel). 2023;10(5)).
I don’t think that capillary filling is quite as useful in preterm infants, kept in incubators, with their immature control of vascular tone, but there is still some correlation between cap filling and blood flow measured by doppler in the SVC. (Osborn DA, et al. Clinical detection of low upper body blood flow in very premature infants using blood pressure, capillary refill time, and central-peripheral temperature difference. Arch Dis Child Fetal Neonatal Ed. 2004;89(2):F168–73). As you can see below there is a lot of scatter, but a higher SVC flow is correlated with shorter CRT.

Combining such clinical signs with the direction of change in serum lactate (the absolute value doesn’t help much in the first couple of days as it is often high after birth), urine output (also not much use immediately after birth), level of activity etc, seems to me to be likely to be important in determining treatment in septic babies also. But we have very few good randomized trials of treatment approaches in septic newborns.
This trial gives us some pointers of how we could reasonably design such a trial, with a structured algorithm of interventions, including clinical pointers and targeted functional echocardiography in some patients, and how to design and analyse the primary outcome. We could develop a consensus algorithm (it couldn’t really be evidence-based) and test against usual care, with a hierarchical composite outcome including death and brain injury and duration of intensive care support, for example.








