There are only a few randomized trials in neonatal surgery, but those that exist have had a major impact. This new publication may do the same, even though the sample size is relatively modest, and there are some issues with the article. You can see some of the difficulties in doing such trials from the fact that it took 12 hospitals 9 years to recruit 80 patients, 58 of which came from only 3 of those hospitals, Sick Kids, GOSH, and University Children’s Hospital in Belgrade, the others having between 1 and 5 patients each. (Eaton S, et al. STAT trial: stoma or intestinal anastomosis for necrotizing enterocolitis: a multicentre randomized controlled trial. Pediatr Surg Int. 2024;40(1):279).
The investigators enrolled infants with NEC prior to surgery, and randomized them during the procedure if they felt that either enterostomy or primary anastomosis were both reasonable surgical options. After elimination of one subject who had been randomized twice, they had 79 patients enrolled, with 42 having a stoma and 37 a primary anastomosis. This appears to be a very reasonable trial approach, where the individual surgeon has equipoise at the moment of surgery.
The first problem with the trial is that there were 6 patients lost “to all follow up”. I don’t understand how it is possible that the authors don’t even know if they survived or not. If there were big problems with record-keeping in some centres maybe the primary outcome variable, ‘days on parenteral nutrition’ might be difficult to find years later. But this was a prospectively registered trial, so it is not clear to me how simple data, easily available during the initial hospitalisation, can be missing on 7% of the subjects.
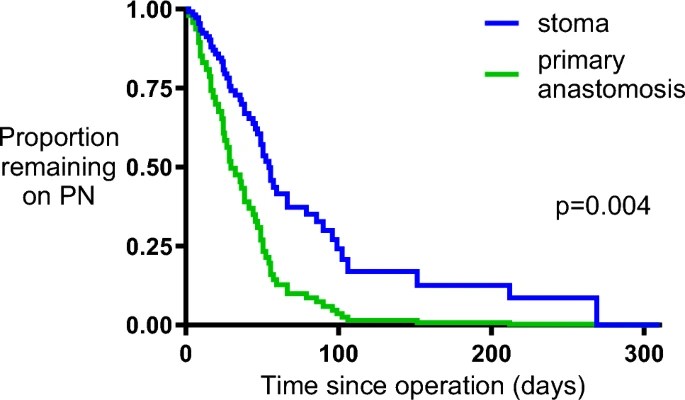
There are other significant problems with the manuscript. The primary outcome was, as mentioned, days on TPN, but how the investigators dealt with mortality in this outcome is not at all clear, the results present the primary outcome among survivors initially, which was a median of 51 days (range 3 days to 4 babies still on TPN at the end of follow up 310 days) among the stoma babies, and 30 days (range 4-105). They then present an analysis by an adjusted Cox regression, censored for mortality. As noted, they state in the text that 4 stoma babies were still on TPN at the end of follow up, but the figure shows everyone as being off TPN before 300 days.
The survival curves are also strange. There were only 4 deaths in the primary anastomosis group, but the curve seems to show about 13 steps down in the survival curve, and both curves continue to show deaths up to 200 days, this isn’t because some patients haven’t yet reached the final follow-up as that was completed in January 2020, and there were no further losses to follow-up in the anastomosis group at 3 months or at 1 year. The curves seem to suggest that the final proportion of the stoma patients surviving was 0.8, but there were 4 deaths of 35 with known outcome, which leaves a proportion of 0.88 surviving.
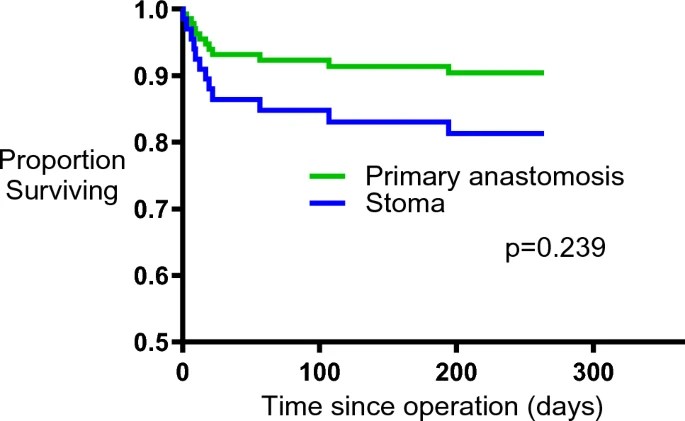
While keeping all of these concerns in mind, the results do seem to show major advantages of primary anastomosis, with the duration of TPN among survivors being shorter, and there being more survivors, 8 deaths in the stoma group vs 4 after anastomosis.
It would be interesting to see whether the experience with the stoma patients in the trial is similar to other patients having a stoma outside of the trial. It seems to me that the fact that 10% of the stoma patients were still on TPN at one year of age, when they were already a selected group, who were relatively stable and with relatively restricted disease, is a surprisingly poor outcome. There were substantially more complications in the survivors in the stoma group, with more wound infections, and, of course, more stoma complications, than among the survivors in the anastomosis group.
The study report may have a lot of big problems, but it does at least suggest that immediate primary anastomosis is a very viable approach in infants who are stable enough to have it considered, and in whom the distribution of disease makes it feasible. There may well be fewer post-op complications with anastomosis, and the number of later strictures were similar between groups.









Hi Keith, thanks for the blog. Just to clear up one simple issue, which is for the graphs. The graphs for a Cox Regression analysis work differently for those on a classic Kaplan-Meier type survival curve. In a Cox analysis, there is a step every time there is a change in the adjusted survival function provided by the multivariate model – so you will notice that every time the primary anastomosis group changes, so does the stoma group. That is also why the mortality and PN curves finish on a different number from those that you might think from the dichotomous raw data – the graphs are model fits rather than the actual raw unadjusted data. We presented these as that was what the statistics presented in the paper but acknowledge thatr this might appear confusing to those expecting a Kaplan-Meier curve.
Best regards,
Simon