It has been clear for a while that the focus of some groups and some publications on only infections associated with central venous catheters, so-called CLABSI, was missing the point. You could completely eliminate CLABSI by not using central lines, but the babies don’t care what the source of their infection is! Also, most serious infections are Gram-negatives, which are largely the result of blood-stream invasion by organisms in the infant’s own GI tract.
When I first moved to Montréal, to take over the NICU at the Royal Victoria Hospital, we had access to the “Usher needle” a tiny butterfly with a side-loop, inserted by the nurses using a forceps to grasp the side loop, often into scalp veins. There were almost no central lines apart from umbilical catheters (as we had to send the babies to the Montreal Children’s for a picc), and therefore very few CLABSI! We did have what I then called nosocomial infections, the name being derived, I think, from the Greek: nosos meaning something to do with infections, and comial meaning… something else, which I guess had to do with health care. I think Hospital Acquired Infections is a better name, and suggests that the hospital is to blame, so I will call them HAI. Hospital Onset Bacteraemia, is a newer terminology, referring only to blood culture positive cases, and is presumably meant to be more neutral, but maybe being neutral isn’t the best idea. Back at the Royal Vic, with the improved survival and prolonged need for vascular access for some infants, and the disappearance of the Usher needle, I developed a central catheter team, which led to a dramatic increase in CLABSI, but no real change in HAI.
If you look at the CNN reports, for many years there have been data on CLABSI, as well as a report of all Late-Onset Infections. The variations in incidence of CLABSI are much greater than of HAI. It is also important to point out that the CNN reports blood culture positive infections. So-called culture-negative sepsis is not included in the main reports; there are guidelines for deciding which cultures may be contaminants, a consideration which, of course, mostly applies to COagulase Negative Staphylococci, or CONS, but those guidelines are somewhat subjective, as always. The CNN report divides the CLABSI into CONS and other organisms, and just under half of the CLABSI are CONS.
Of the remainder, the majority, as mentioned above, are probably primarily organisms invading from the GI tract of the baby, a few recent publications seem to confirm this. Using the latest metagenomic techniques, (Schwartz DJ, et al. Gut pathogen colonization precedes bloodstream infection in the neonatal intensive care unit. Sci Transl Med. 2023;15(694):eadg5562), with sequencing of multiple stools from 19 preterm infants with HAI, they showed that prior to the development of sepsis with Gram negative organisms or with Enterococci, there was an extremely high relative abundance of the organism in the GI tract, of over 10% in all, and sometimes reaching over 45% of all the bacteria in the gut being the offending germ that went on to cause the bacteraemia. In contrast, babies with Staph Aureus sepsis or with late-onset Group B Strep, had very little of the organism in the stool, except one S Aureus baby with >90%. Which seems to confirm that Enterobacteriaceae and Enterococci sepsis is usually due to blood stream invasion by GI organisms, whereas the other bugs mentioned usually come from elsewhere, probably the skin or pharynx, or from the skin of the health-care team.
Another recent publication, this time from Singapore, (Heston SM, et al. Strain-resolved metagenomic analysis of the gut as a reservoir for bloodstream infection pathogens among premature infants in Singapore. Gut Pathog. 2023;15(1):55) also showed that Enterobacteriaceae causing HAI (with close to 100% DNA identity) were previously found in the GI tract, whereas the S Aureus and 2 of their 4 late-onset GBS were not found.
The team from St Louis have also previously confirmed that giving antibiotics increases the presence of pathogens, and, in particular antibiotic resistant pathogens, in the GI tract of preterm infants in the NICU (Gibson MK, et al. Developmental dynamics of the preterm infant gut microbiota and antibiotic resistome. Nat Microbiol. 2016;1:16024).
Central venous catheters are not, therefore, a frequent source of HAI in preterm infants, low gestational age is the major risk factor, prolonged initial antibiotics, and not receiving probiotics are all as important as risk factors in our population. Indeed just being in the NICU, which has it own microbiome and which interchanges with the infant’s microbiome, is a major risk. A study from a few years ago showed that the highest bacterial abundance was on the floor of the NICU room, just in front of the incubator, (Brooks B, et al. The developing premature infant gut microbiome is a major factor shaping the microbiome of neonatal intensive care unit rooms. Microbiome. 2018;6(1):112) and that there appears to be a dynamic interchange between the infant’s bowel microbiome and the local environment. Brooks B, et al. Strain-resolved analysis of hospital rooms and infants reveals overlap between the human and room microbiome. Nat Commun. 2017;8(1):1814.
Scrupulous technique for insertion and care of central venous lines is essential for any patient with such a catheter. But even the best quality control of catheters will probably not have much overall impact on HAI incidence, unless there are also evidence-driven interventions to reduce other sources of HAI.
This post is actually in response to a recent publication from the Pediatrix group, and 5 other academic NICUs, Prochaska EC, et al. Hospital-Onset Bacteremia Among Neonatal Intensive Care Unit Patients. JAMA Pediatr. 2024;178(8):792-9) which reflects a change in the USA, where the CDC is introducing HAI, specifically bacteraemia with an onset more than 3 days after admission, which is called Hospital Onset Bacteraemia, or HOB, as a quality metric. The publication documents the HOB frequency per 1000 patient days:
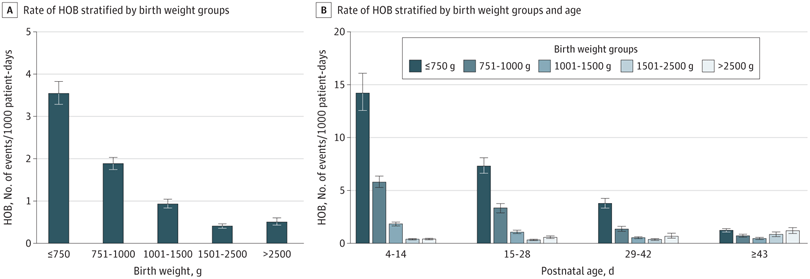
As the second graph shows, HAI become less frequent with postnatal age among the very preterm, but become more frequent over time in the term babies. Obviously most term babies who are still in the NICU after 1 month of age are very complex babies with multiple problems:

whereas among the very preterm, they are becoming more stable over time, as well as having progressively more mature immune systems. Presence of a central line is a good marker of these changes, any baby still needing a central line after 6 weeks of age is at very high risk of HAI.
In older patients, some definitions of a true CLABSI require paired quantitative cultures, with a greater CFU concentration in the culture drawn from the line than from a peripheral site. We almost never do that, mostly for technical/logistic reasons (blood volume and risk of catheter occlusion), so definitions of CLABSI are somewhat variable, and not necessarily directly comparable. In the CNN the definition is simple, a positive culture with a central line in place, or within 48 hours of withdrawing the line; I think it is obvious that many such bacteraemias are not due to central line contamination. Recording any positive blood culture, with some filters to eliminate contaminants, is simpler, more likely to be comparable, and is more relevant for the lives of our babies. As one example of how this is pertinent, one site in the CNN 2022 annual report had the highest crude rate of HAI for infants <33 weeks at 6.6/1000 patient days, but had one of the lowest incidences of CLABSI (4/1000 central line days, of which 1.4 were CONS).
We need to focus on maintaining scrupulous had hygiene, limiting unnecessary antibiotics, and trying to manipulate the intestinal microbiome to reduce or eliminate pathogens. Other interventions, attempting to support the immature immune system (IV immune globulin, Colony Stimulating Factors, neutrophil transfusions) have so-far proven ineffective. As the JAMA Pediatrics article shows clearly, HOB are a substantial cause of mortality, fighting them is a priority.








