In a newly published trial (Roze JC, et al. Prophylactic Treatment of Patent Ductus Arteriosus With Acetaminophen: A Randomized Clinical Trial. JAMA Pediatr. 2026) nearly 800 infants of 23 to <29 weeks GA were randomized within 12 hours of birth. There were few exclusions, basically only congenital anomalies and Twtin-Twin transfusion syndrome. The doses were different among the 27-28 weeks infants compared to those more immature, and continued for 5 days in both groups.
The primary outcome variable was survival without “severe morbidity” which was any one of : severe bronchopulmonary dysplasia, stage II or III NEC, grade III or IV IVH, or cystic leukomalacia. Severe BPD used the 2018 NIH consensus definition, i.e. invasive ventilation with more than 21% O2, or CPAP with more than 30% O2, or high flow at more than 3 lpm. Outcome was determined at 36 weeks or discharge home.
There was no outcome difference of importance between the groups, as you can see below.
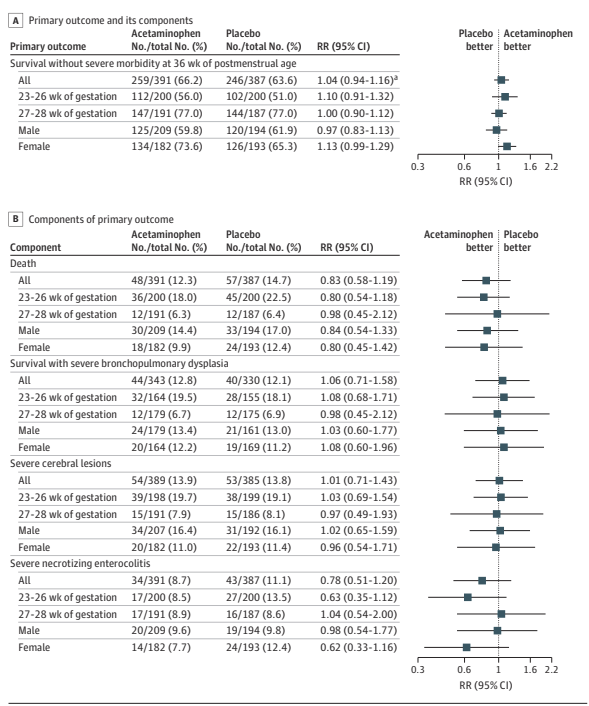
I don’t know why they inverted the groups between part A and B of the figure, which misled me briefly, as you can see there is a minor difference in NEC in the most immature infants, and among females, but this may well be a random variation.
It is also revealing that Acetaminophen was not very effective at closing the PDA :
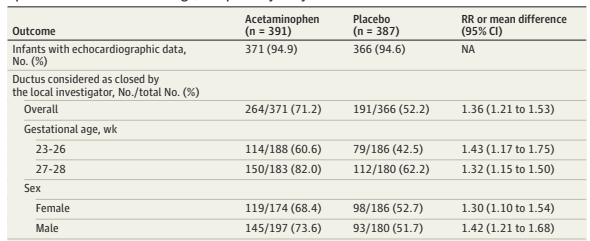
Among babies who had an echocardiogram at 7 days of age, the rate of PDA closure was 43% in the more immature controls, and 61% with active medication. In comparison, prophylactic ibuprofen seems probably a little more effective for PDA closure; the Cochrane review of prophylactic ibuprofen shows closure of the PDA on day 3 to 4 of life of 58% in the controls compared to 83% with ibuprofen, from meta-analysis of 9 studies with a total of about 1000 babies.
21% of controls and 14% of acetaminophen infants had medical PDA “backup” treatment, which started a median of 7 days after birth, with a 1st quartile of 3 days. So, many of those “back-up” treatments started during the initial randomization period. A total of around 3% in each group had, eventually, formal closure (surgical or catheter) of the PDA.
The more immature GA stratum had the poorest response to acetaminophen, but still had many more PDAs closed at 7 days of age with acetaminophen than placebo. Apart from numerically fewer cases of NEC in this subgroup, with 95% confidence intervals which include no difference, there is no apparent difference in outcomes, either in the components of the primary or any of the secondary outcomes. Among the secondary outcomes, in the more immature group, there were also numerically fewer pulmonary haemorrhages, 4.5% vs 8%, and fewer babies who had catecholamine support or postnatal steroids in the first 7 days. But again, for all of these findings, the confidence intervals include no difference.
This trial confirms what we have been seeing in many recent studies. There is no advantage to routine PDA closure. There are still those who seem certain that there are some PDAs that should be closed in small preterm infants. My response remains that it may be true, but we really need a way to define that subgroup of infants, and then find the most effective, least toxic way of closing their PDA.








